The differentiation of mammalian red blood cells in bone marrow (a process called erythropoiesis) is one of the most striking examples of specialization occurring in nature.
In adults, erythropoies is begins with a pluripotent (i.e., multi-potent) stem cell that gives rise in 7 to 10 days to mature, hemoglobin-filled erythrocytes.
Differentiation and specialization of cells may be accompanied not only by the acquisition and development of specialized structures but also by the loss of internal structures or physiological properties.
The latter is the case during erythrocyte differentiation, for mature red blood cells lack nuclei, mitochondria, endoplasmic reticulum, Golgi bodies, ribosomes, and most other typical cell organelles.
The mature erythrocyte is a relatively simple cell, delimited at its periphery by a plasma membrane and containing internally a highly concentrated, paracrystalline array of hemoglobin molecules used for oxygen transport.
The apparent simplicity of the maturing erythrocyte is the principal reason for its selection over most other kinds of cells as the preferred object for studying plasma membrane structure and protein (e.g., hemoglobin) structure and biosynthesis. These subjects, together with the contributions made by intensive study of the erythrocyte.
Erythropoiesis:
The’ development and differentiation of the mammalian red blood cell is depicted in Figure 24-7. Development takes place in the extra-sinusoidal stroma of the bone marrow and begins with pluripotent stem cells capable of proliferating leukocytes (white blood cells) as well as erythrocytes.
When primitive stem cells undergo division, one of the daughter cells remains undifferentiated and pluripotent, so that depletion of marrow stem cells does not normally take place. The erythropoietic activity of the bone marrow is under hormonal influence, increasing or decreasing according to the level of circulating erythropoietin (produced in the cortical region of the kidneys and secreted into the bloodstream).
The erythrocyte progenitors show an increasing sensitivity to erythropoietin through the proerythroblast stage and a parallel, ever- decreasing proliferative potential (Fig. 24-8). As a result, by the proerythroblast stage, the cells are irreversibly committed to the maturation sequence leading to erythrocytes.
The mRNAs for the various globin chains of hemoglobin appear and increase in quantity in the proerythroblast and erythroblast stages, and this is followed by the synthesis and accumulation of hemoglobin. By the late erythroblast and normoblast stages, the synthesis of hemoglobin accounts for more than 95% of all protein synthesis occurring in the cells.
Hemoglobin synthesis is concluded in the reticulocyte stage and is accompanied by the progressive dissolution of internal cell structure (including the loss of the nucleus) and residual nucleic acids. Late reticulocytes leave the bone marrow and enter the circulating blood, where in the ensuing hours they lose their granulation and are transformed into the biconcave disks typical of mature erythrocytes. Complete differentiation and maturation from stem cell to the erythrocyte takes from 7 to 10 days.
Because of its highly differentiated state, the mature erythrocyte is incapable of further proliferation. In humans, the average life span is 120 days. As there are 5 billion red blood cells in each cubic centimeter of blood, a few simple calculations quickly reveal that in a typical adult the differentiation and maturation of 3 million erythrocytes is completed each second! Obviously, an appreciable proportion of the body’s energy and resources is continuously consumed to support erythropoietic activity. This is in stark contrast with other highly differentiated cells such as those of muscle and nerve, whose proliferation ceases shortly after birth.
Genetic and Molecular Basis of Erythrocyte Differentiation:
Because of the intensity with which the red blood cell has been studied by biochemists, cell biologists, molecular geneticists, physiologists, and others, the differentiation and specialization of this cell are better understood in molecular terms than any other; accordingly, erythrocyte differentiation may serve as a model for the genetic and molecular events that underlie cell differentiation generally.
Development in humans is accompanied by the sequential appearance of six different hemoglobin’s composed of various combinations of seven different globin chains. The structural genes coding for these chains represent only a minuscule fraction of the total genetic complement of the pluripotent progenitor cells. In humans, there are two pairs of alleles (i.e., four genes) for alpha globin chains, one pair for beta chains, two pairs for gamma chains, one pair for delta chains, one pair for epsilon chains, and two pairs for zeta chains.
These genes account for less than 0.0002% of the total DNA content of the nucleus, and yet globin chain synthesis accounts for more than 95% of all protein synthesis taking place in the red cell by the later stages of maturation. It is clear that during differentiation, the progeny of the stem cells are committed to the highly selective expression of only a small number of genes.
The globin chain genes are distributed between two pairs of homologous chromosomes—alpha and zeta chain genes on one chromosome pair and beta, gamma, delta, and epsilon chain genes on the other pair. The zeta, epsilon, and gamma chain genes are expressed only during embryonic and fatal development, whereas the beta and delta chain genes are expressed from mid-fetal stages through adulthood.
Alpha chain genes are expressed throughout life beginning at an early embryonic stage. Therefore, superimposed on the highly selective expression of globin chain genes in maturing erythrocytes is the temporal expression of certain members of this family of genes during organismal development. Expression of these genes is also coordinated between the two different chromosomes bearing the members of this gene family.
A most interesting finding of recent years is that the order in which the globin chain genes are arranged on their respective chromosomes parallels the order in which the various genes are expressed during embryonic and fetal development.
Also present in the chromosome regions containing these genes are nucleotide sequences encoding polypeptide chains that are very similar in primary structure to the globin chains, but that are never expressed. These “silent genes” or pseudogenes may be genetic vestiges of the evolutionary process. Certainly, the inclination to draw a parallel between phylogeny and ontogeny at the organismal and cellular levels is unavoidable.
Cellular DNA includes not only structural genes but also sequences vital to DNA organization within the chromosomes and the coordination of gene expression during differentiation. About 60% of all the nucleotide sequences in the DNA of stem cells belong to the “unique sequence” class in which only a few copies of each sequence are present.
The structural genes for the globin chains belong to this class. Highly repetitive DNA accounts for about 10% and consists of short sequences repeated in tandem many thousands of times. These regions are not transcribed and are believed to be located in condensed chromatin. The balance of the DNA-about 30%-is moderately repetitive (repeated up to several hundred times) and includes the genes for histones and the ribosomal RNAs.
Some moderately repetitive DNA sequences are located adjacent to the structural genes for globin and other proteins and may be involved in the coordination of gene activity. For example, by binding to the moderately repetitive sequence, regulatory substances could “turn on” the transcription of physiologically related genes.
In the case of the red blood cell, such a gene set would be represented by:
(1) The globin chain genes,
(2) The genes for the heme synthetic enzymes, and
(3) The genes for the cell surface antigens (which serve as the basis for blood typing).
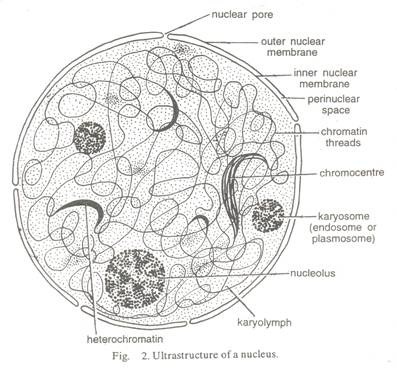
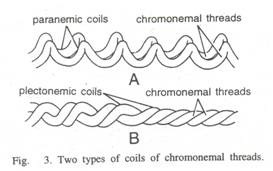
The genes of eukaryotic cells are associated with histones and other basic proteins to form chromatin, which is composed of repeating nucleosome units. Euchromatin has the more open structure and is transcriptionally active, whereas the condensed heterochromatin is not transcribed.
Experiments with developing erythrocytes indicate that the globin chain genes are included in nucleosomes of condensed chromatin during the early stages of differentiation and that these are converted to the open form just before globin mRNA synthesis begins. The transcription of globin DNA sequences by RNA polymerase II that occurs when these genes are “turned on” can be traced to a modification of the associated histones and an interaction with non-histone proteins.
A selective expression of globin mRNA genes occurs in erythroblasts, with the result that globin mRNA is produced in amounts 100 times greater than expected on the basis of the proportion of total template DNA represented by the globin genes. Globin chain synthesis parallels the appearance of globin mRNAs in erythroblasts.
Although globin chain synthesis accounts for the overwhelming majority of all protein synthetic activity in the maturing erythrocyte, a number of other structural genes are expressed (e.g., those for the enzymes of glycolysis, enzymes for initiation, elongation, and termination of globin chain assembly, enzymes of the metabolic pathway for heme synthesis, enzymes and structural proteins of the plasma membrane, and so on).
Although all protein synthesis comes to a halt during reticulocyte maturation, a red cell retains a limited metabolic capacity after release from the bone marrow. For example, glycolytic activity provides the ATP needed to maintain the sodium and potassium pumps of the erythrocyte membrane and for other energy-requiring processes. What limited metabolism is retained by the mature cell serves to sustain it during its 120-day and 700-mile journey through the circulatory system.
The progressively selective expression of genes in the maturing red blood cell is accompanied by the loss of internal structure so that in the mature state the only remaining organelle is the plasma membrane itself. Internally, the cell consists primarily of a highly concentrated (30% by weight) crystal like arrangement of hemoglobin molecules suited to the cell’s principal function—oxygen transport.
Morphological and Physiological Specialization of Red Blood Cells:
Little cell growth occurs during the periods between the successive mitotic divisions of erythropoiesis. As a result, the mature erythrocyte is among the smallest cells of the body. In humans, the average red blood cell has a volume of only about 100 µm3. The natural shape of the cell is that of a biconcave disk (Fig. 24-9), although the cell is flexible and its shape is easily distorted when the cell passes through narrow capillaries. The factors that maintain this rather unusual cell shape have fascinated scientists for more than two centuries.
Prior to the discovery of the existence of cytoskeletons, the prevailing hypothesis suggested that the biconcave shape resulted from the chemical nature, arrangement, and interaction of the protein and lipid molecules that comprised the plasma membrane.
However, it is now apparent that the biconcave shape is due to the modest cytoskeleton lying just beneath the plasma membrane. Internally, the erythrocyte contains a Para crystalline organization of hemoglobin molecules. Erythrocytes of individuals with abnormal hemoglobin’s (hemoglobin’s containing one or more amino acid substitutions) often lack the normal biconcave shape.
The most notorious example is the “sickle” or crescent shape of erythrocytes in individuals with sickle-cell anemia. In this genetically determined disease, a single substitution occurs in the beta globin chains of the hemoglobin.
Under conditions of oxygen deprivation or shortage, the hemoglobin molecules aggregate to form long fibers and these progressively group together into bundles. The bundles of hemoglobin molecules make the cells less flexible and eventually overcome the constraints of the cytoskeleton, deforming the cells and causing their sickling.
Oxygen enters and leaves the erythrocyte by diffusion and the biconcave shape facilitates oxygen flux by increasing the surface area-to-volume ratio of the cell. Oxygen inside the cell forms a reversible combination with hemoglobin, binding to hemoglobin as the blood circulates through the capillary networks of the lungs (where the net oxygen flux is directed into the erythrocyte) and being released as the blood circulates through oxygen-deficient tissues.
The disk shape of the erythrocyte induces the formation of rouleaux or long stacks of cells, with the result that far greater numbers of cells can pass through the narrow capillaries when arranged in such a regimented manner than when the cells are freely and independently suspended. Experimental elimination of the biconcave shape using hypotonic solutions eliminates the capability of erythrocytes to form rouleaux.