The following points highlight the three main mediums of Identification of Bacterial Growth. the mediums are: 1. Growth on Nutrient Agar 2. Blood Agar 3. MacConKey’s Agar.
Contents
Medium # 1. Growth on Nutrient Agar (Table 7.2):
Steps to be adopted:
1. Observe and record the morphology of colony and pigment production in nutrient agar plate or tube. To identify a bacteria by its colonial morphology only, may not be enough. So a battery of other relevant tests is to be undertaken.
However, pigment production, if present, may give some clue. Generally, bacterial growth with green pigment on nutrient agar is supplied. Pigment is diffusible in the medium in case of pigmented Pseudomonas (Fig. 7.2) whereas Staphylococcal pigment remains localised within the bacterial colony (Fig. 7.1), e.g. golden-yellow pigment in Staph, aureus and white pigment in Staph, epidermidis.
In liquid medium like peptone water, greenish pigment may also be present with surface pellicle formation. Surface pellicle (e.g. in cases of vibrio and Bacillus) indicates strong aerobic nature of bacteria as more oxygen is available near surface.
2. Examine Gram’s stained smear and hanging drop preparation.
Record your findings:
(i) Gram staining:
(a) Gram-negative rods
(b)Gram-positive cocci in clusters (Staphylococci)
(c) Gram-positive rods with or without spore
(ii) Hanging drop:
(a) Motile rods
(b) Non-motile cocci rod
Findings:
The findings are recorded and Tables 7.3, B, C, G & H are followed to arrive at identity.
Growth on Any Other Special (Selective/Inhibitory/Indicator) Medium:
Any growth on special selective/indicator/ inhibitory medium is to be identified by undertaking the following steps:
1. Identify the medium and think the bacteria which grows on it.
2. Note the colony character and any indicator of growth for any special genus, e.g., sucrose fermenting flat yellow colony on T.C.B.S. agar indicates growth of vibrio.
3. Perform morphological study by gram stain or any special stain (eg. capsule staining, spore staining, Wayson’s staining for Y. pestis etc.).
4. Perform motility.
6. Go for biochemical tests.
7. Tests for enzyme and toxin production.
8. Antigen detection by slide agglutination or capsule swelling using specific high titre sera (HTS).
a. Pseudomonas Aeruginosa:
Pathogenicity:
The organisms produce blue pus and pyocyanea literally means “blue pus”. Ps. aeruginosa is an important cause of hospital-acquired infection. Most infections occur in patients with serious underlying diseases like burns and malignancy or as a result of therapeutic procedures (catheterisation, cystoscopy). Prior treatment with antimicrobials favour pseudomonas infection.
1. Skin infections especially in wound, pressure sores and burns.
2. Urinary infection, usually following catheterisation or in chronic infections.
3. Respiratory infections, especially in immunosuppression and cystic fibrosis.
4. Ear infections, e.g. chronic otitis media and otitis externa.
5. Eye infections, usually hospital acquired.
6. Septicaemia may develop in neonates and old debilitated persons, particularly in patients receiving cytotoxic drug or irradiation.
7. Acute necrotising vasculitis which leads to haemorrhagic infarction of skin (ecthymagangrenosa) and of internal organs (liver and kidney).
Laboratory diagnosis:
Specimens:
Pus, wound swab, mid-stream specimen of urine, CSF, sputum or blood.
Culture:
On MacConkey’s agar they show pale, flat colonies with a spreading border. In nutrient agar or Mueller-Hinton agar there is diffuse bluish, greenish or reddish brown pigments, and a grapelike or fruit-like odour. Selective media such as cetrimide agar is useful for isolation of the organism from faeces or other samples contaminated with mixed flora.
Identification is made based on:
1. Characteristic colony morphology and gram- film appearance.
2. Grape-like or fruit-like odour of the colony.
3. Mucoid colony variants are particularly prevalent in respiratory tract specimens.
4. Biochemically, P. aeruginosa is confidently identified based on the following features:
(a) Positive oxidase test (Table 7.10).
(b) Triple sugar iron (TSI) agar reaction of alkaline over no change.
(c) Bright green diffusible pigments on Mueller-Hinton or other non-dye-containing agars (e.g. N. agar).
(d) Growth at 42°C.
Occasional strains of P. aeruginosa produce only pyoverdin, which would not differentiate them from P. fluorescens or P. putida. These latter species fail to grow at 42°C, while P. aeruginosa grows at 42°C.
b. Staphylococcus (S.aureus):
Pathogenicity:
S. aureus is an important pyogenic organism and Box 1 shows the important diseases produced by the same.
Laboratory diagnosis:
Specimens:
These are to be collected depending on the nature of lesion, pus from suppurative lesions, CSF from meningitis, blood from septicaemia, sputum from respiratory infection and suspected food, vomit or faeces from food poisoning.
1. Smear:
Examination of a Gram-stained smear of pus and other specimens shows Gram-positive cocci in clusters with some single and paired cocci.
2. Culture:
(a) Specimens are inoculated on blood agar or selective agar medium with 7% sodium chloride which inhibits the growth of most organisms other than staphylococci.
(b) Mannitol salt agar is selective and differential media for staphylococci. Mannitol is fermented by S. aureus but not most other staphylococci.
3. Identification:
(a) Coagulase test: S. aureus is coagulase positive.
(b) Antibiotic susceptibility tests, biochemical profiles (bio-typing), phage typing, nucleic acid analysis may be done for the intra-species identification of the organism for epidemiological study to trace the source of staphylococcal infections.
c. Bacillus:
Members of the genus Bacillus are aerobic, spore- bearing, gram-positive bacilli arranged in chain. The spores are retractile, oval and central in position and its diameter is the same as the width of the bacteria.
Bacillus anthracis:
Species:
I. Pathogenic:
(a) B. anthracis — causative agent of anthrax.
(b) B. cereus — cause food poisoning.
II. Non-pathogenic (saprophytes):
(1) Large-celled: B. megaterium, B. cereus
(2) Small-celled: B. subtilis, B. stearothermophilus
Pathogenicity:
Anthrax is a zoonosis, humans are occasionally secondarily infected from diseased animal or animal products.
Anthrax is of 4 clinical types:
(1) Cutaneous anthrax:
Spores enter the skin most commonly through abraded skin, crusts or hair follicles and usually produce a single painless blister, often called ‘malignant pustule’.
(2) Intestinal anthrax:
Ingestion of contaminated meat results in severe and often fatal form of gastroenteritis which is far less common than cutaneous form.
(3) Pulmonary anthrax:
It is often referred to as ‘wool-sorter’s disease’ and is caused by inhalation of large number of spores and is usually fatal. It is a rare form of anthrax in developing countries.
(4) Septicaemia anthrax:
Cutaneous intestinal and pulmonary anthrax, if not treated in time, progress into septicaemia and death occurs from overwhelming infection.
Laboratory diagnosis:
Specimens: Pus, fluid, sputum or blood depending on the type of lesion. Specimen must be labelled “High Risk”.
Microscopy:
B. anthracis is capsulated, non-motile, large (5-8/1.5 μm), gram-positive rod with square ends. Spore forms never occur in tissues but develop after the organism is shed or if it is grown on artificial media. Spores can be stained by modified Ziehl- Neelsen’s method. Capsules are formed in the tissues but are usually lacking in culture.
McFadyean’s reaction:
When B. anthracis in blood of animals in a heat fixed film is stained with polychrome methylene blue for 10-20 seconds, disintegrated capsular material appears amorphous and purplish around the bacilli.
Culture:
B. anthracis is aerobe and facultative anaerobe, grows readily on ordinary media over a wide-range of temperature (25°-30°C), optimum 35°C. Colonies are 2-5 mm in diameter, dense, grey-white; they are composed of parallel chains of cells producing wavy margin of the colony, the so-called ‘Medusa head’ or ‘curled hair lock’ appearance.
1. Blood agar:
Colonies are non-haemolytic or only slightly haemolytic (saprophytic Bacilli species are markedly haemolytic).
2. Nutrient broth:
Growth is not usually turbid but forms a thick pellicle on the surface.
3. Gelatin stab culture:
Growth occurs along the tract of inoculating wire with lateral spikes, widest near the surface — the “inverted fir tree” appearance, but the liquefaction is late.
Animal inoculation:
When white mouse or guinea pig is intra-peritoneally inoculated with a small amount of exudate or, culture, the animal dies in 36-48 hours. Heart blood and sputum shows B. anthracis.
Bacillus subtilis:
It is a non-pathogenic saprophyte and appear as common contaminant of specimen and laboratory media.
Laboratory diagnosis:
Culture:
Nutrient agar shows dry, 2-3 mm greyish-white opaque colonies. In nutrient broth, there is uniform turbidity.
Gram-staining:
Gram-positive bacilli with sub-terminal spore.
Animal pathogenicity:
Non-pathogenic to laboratory animals. They also differ from B. anthracis in producing β-lactamase which is different from that produced by staphylococci and are motile.
Medium # 2. Blood Agar:
a. Streptococcus:
Streptococcus is a gram-positive coccus arranged in chain.
Classification:
A. Haemolytic classification:
Preliminary classification of streptococci is made based on the type of haemolysis produced on blood agar plates.
(i) β-haemolytic streptococci:
They produce a wide (2-4 mm wide) clear zone of complete haemolysis around the colony (Fig. 7.8).
(ii) α-haemolytic streptococci:
They produce a partial haemolysis (1-2 mm wide) with greenish discolouration. Some un-haemolysed RBCs are detectable in the haemolytic zone. Alpha haemolysis is seen in pneumococcus and viridans streptococci.
(iii) γ-haemolytic streptococci:
They produce no haemolysis and Streptococcus faecalis is a typical member.
B. Serological classification (Lancefield and Griffith classification):
The β-haemolytic streptococci are classified by Lancefield (1933) serologically into a number of broad groups on the basis of group specific polysaccharide antigen of cell wall. To date, 20 Lancefield groups have been identified, numbered A-V (without I and J) by precipitation reaction with appropriate sera. Majority of the human pathogens belong to group A which are also called Streptococcus pyogenes.
The strains of group A streptococci are further subdivided by type specific antisera into 80 Griffith serotypes (type 1, type 2, etc.) according to their surface proteins (M, T and R). M protein is most important type specific antigen which exists in approximately 80 antigenic forms, each of which is present in a different serotype of S. pyogenes.
Streptococcus pyogenes:
Pathogenicity:
Box 2 shows the important lesions produced by different species of streptococci.
Laboratory diagnosis:
A. Acute suppurative infections:
Specimen is collected from the site of lesion such as swab, pus or blood depending on the nature of infection, such as swabs taken from throat, vagina or purulent lesion of patients and from the throat and nose of suspected carriers.
1. Smears:
Microscopy of smears of pus showing Gram-positive spherical or oval cocci in chains or pairs in association with pus cells suggests the presence of streptococci (Fig. 7.7). Non-viable organisms are gram-variable.
2. Culture:
Specimen should be inoculated immediately or sent to the laboratory in Pike’s transport medium (blood agar containing 1 in 1,000,000 crystal violet and 1 in 16,000 sodium azide). Specimen is inoculated in blood agar medium and incubated at 37°C overnight. Haemolysis develops better under anaerobic conditions or under 5-10% carbon dioxide.
Sheep blood agar is preferable as human blood may contain inhibitors. The bacterial colonies are small, typically matt or dry and surrounded by β-haemolysis. Haemophilus haemolyticus produces colonies resembling those of β-haemolytic streptococci but their haemolysis is inhibited by sheep blood. Hence primary isolation should be done in sheep blood agar.
Serological testing for determination of Lance- field group and Griffith type of haemolytic streptococci is done when needed for definite classification and for epidemiological study.
A simple technique of detection of S. pyogenes (group A) is done by agar plate test using paper discs impregnated with bacitracin. S. pyogenes is more sensitive to bacitracin than other streptococci. Selective media like crystal violet blood agar that inhibits throat commensals and may facilitate the detection of small numbers of S. pyogenes in throat swabs, but are rarely used in routine culture.
3. Antigen detection tests:
Commercial test kits of ELISA, and agglutination tests are now available to demonstrate group A streptococcal antigen from throat swabs which are 75-80% sensitive.
Commercial test kit of a nucleic acid probe-based test for direct detection of group A streptococci in throat swabs is available.
4. Serological tests:
Although antibodies to most toxins and enzymes of group A streptococci are produced, these antibodies appear late, hence test for antibodies is not helpful in diagnosing acute infection. They are more commonly used to diagnose non-suppurative complications.
B. Non-suppurative complication:
Culture of throat swab or pus from skin lesions helpful for checking the continuing presence of S. pyogenes in throat or impetigo. Serological tests provide evidence of recent streptococcal infection. A rising titre of antibodies to group A streptococcal antigens are usually detectable. ASO titre of 200 units or more is significant in rheumatic fever.
ASO titre is usually found in high levels in respiratory disease and rheumatic fever; but in streptococcal skin infections and acute glomerulonephritis, ASO titre tends to be low and DNase-B test is more reliable. Complement (C3) level is also reduced in serum in acute post-streptococcal glomerulonephritis.
b. Proteus, Morganella, Providencia:
Classification:
Habitat:
Human and animal intestine. Some species are saprophytes and are found in soil, sewage and water.
Pathogenicity:
P. mirabilis is the most important, other species are occasionally encountered in human lesions.
1. Urinary tract infection, especially following catheterization or cystoscopy.
2. Sepsis: Abdominal, wound and middle ear infections. The organisms are generally low grade pathogens and often are secondary invader of ulcers, pressure sores, burns and damaged tissues.
3. Septicaemia.
Laboratory diagnosis:
Specimen:
Depending on the site of infection, which include urine, pus, blood.
Microscopy:
These are actively motile, non-capsulate, gram- negative pleomorphic bacilli.
Culture:
Proteus species grow well on routine media (nutrient agar, blood agar) with a swarming type of growth. This makes the isolation of other bacteria difficult in mixed cultures because swarming from a single colony of Proteus may cover the whole plate culture.
However, swarming is inhibited in media containing bile salts, sewage. MacConkey agar, DCA and XLD agar. Swarming is also inhibited by increasing agar concentration (2%), chloral hydrate (1:500) and boric acid (1:1000) by incorporating in the media.
Colonies:
Colourless, non-lactose fermenting on MacConkey agar. Proteus cultures have a distinctive smell (fishy/seminal).
In a mixed culture, pathogen can be separated from Proteus contaminated plate by sub-culturing in MacConkey agar. Swarming is not exhibited by the Morganella and Providencia.
Biochemical reaction:
Table 7.9 shows the distinctive biochemical characters of the three genera.
1. Lactose is not fermented by any of the three genera, hence colonies are pale on MacConkey or DCA.
2. All produce indole except P. mirabilis, and only two members (P. mirabilis and P. vulgaris) produce H2S.
3. All members produce phenylalanine deaminase and deaminate phenylalanine to phenyl pyruvic acid (PPA).
4. Production of urease and hydrolysis of urea is another characteristic of all members of the group except P. stuartii which is urease-negative.
Differentiation from the common pale colonies of pathogens isolated on lactose containing media is made by testing urease activity. Shigella and Salmonella do not produce urease.
Serology:
Certain antigens (alkali-stable fraction O) of Proteus strains (0 x 19, 0 x K and 0 x 2) are common to Rickettsial prowazekii and agglutinate with sera from patients with rickettsial disease. This antigen sharing forms the basis of Weil-Felix reaction (heterophile agglutination test).
Citrobacter, Enterobacter, Serratia:
Citrobacter, Enterobacter and Serratia species are Gram-negative motile rods and opportunistic pathogens.
Habitat:
They are found in intestinal tract of man and animal, and in soil, sewage and water.
Culture:
These members grow well on routine media such as MacConkey agar, blood agar and nutrient agar.
Biochemical tests:
Citrobacters are late or non- lactose fermenters and enterobacters are lactose fermenters. Serratia is a non-lactose fermenting organism. Some strains of Serratia produce red pigment.
Medically important species include C. freundii, E. aerogenes, E. cloacae and S. marcescens.
Pathogenicity:
1. Urinary tract infection.
2. Wounds, skin lesions and respiratory infections in hospitalized patients.
3. Septicaemia: Some are responsible for outbreaks of infection in nursery, ICU and burns units. They are often multi-drug resistant.
Medium # 3. MacConKey’s Agar:
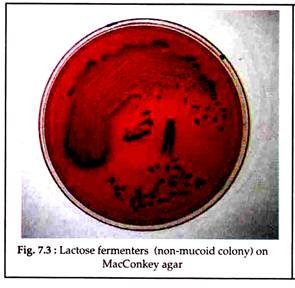
I. Lactose Fermenters:
a.Enterobacteriaceae:
Classification:
The classification of Enterobacteriaceae is complex and controversial. There has been successive changes in the nomenclature of taxonomy with DNA homology studies. More than 30 genera and 120 species or groups have been defined, about 96% of the medically important isolates belong to 14 genera and constitute 38 species.
The oldest method of classification of enteric bacilli is based on lactose fermentation and members fermenting lactose are called lactose fermenters or coliforms.
b. Escherichia Coli:
The main species of medical importance is Escherichia coli which are gram-negative motile bacilli.
Habitat:
E. coli is a normal inhabitant of intestinal tract of humans and animals.
Pathogenicity:
I. Sepsis:
UTI, wound infection, peritonitis, biliary tract infection, septicaemia, neonatal meningitis.
II. Diarrhoea:
Infant gastroenteritis (EPEC), travellers’ diarrhoea (ETEC), haemorrhagic diarrhoea (VTEC) (haemorrhagic colitis, haemolytic uraemic syndrome).
I. Sepsis:
E. coli is an important cause of sepsis:
(a) Urinary tract infection including cystitis, pyelitis and pyelonephritis.
(b) Wound infections, appendicitis, peritonitis, biliary tract infection.
(c) Septicaemia.
(d) Neonatal meningitis.
II. Diarrhoea:
Despite being a normal gut flora, four pathogenic groups of E. coli are recognised that cause diarrhoea.
(a) Enterotoxigenic E. coli (ETEC):
E. coli produces either one or two plasmid mediated enterotoxins, heat-labile enterotoxin (LT) and heat-stable enterotoxin (ST).
LT stimulate adenyl cyclase in mucosal cells of small intestine, which, in turn, activates cyclic adenosine monophosphate (cAMP) that causes hyper secretion of fluid and electrolytes into the intestinal lumen and produces watery diarrhoea. In contrast, ST appears to activate guanylate cyclase and cause diarrhoea.
(b) Enteroinvasive E. coli (EIEC):
The EIEC are far less pathogenic than ETEC and invade the mucosa of colon and cause a dysentery like shigella dysentery in all age groups. They are non-motile and resemble shigella strains in their biochemical reaction (NLF). Important serogroups are O 124 and O 164.
(c) Enteropathogenic E. coli (EPEC):
EPEC is an important cause of outbreak of infantile gastroenteritis in developed countries.
(d) Verocytotoxigenic E. coli (VTEC):
VTEC are named so because of the cytopathic effect of their toxins on vero-monkey kidney cells. There are two antigenically distinct verocytotoxins — VT-1 and VT-2. Commonest VTEC is a serogroup O 157 that causes haemorrhagic colitis and haemolytic uraemic syndrome in children.
Laboratory diagnosis:
Specimens:
Depending on the site of infection specimens are collected which include urine, pus, blood and stool. In case of diarrhoeal diseases, faeces may be examined for toxin detection.
Microscopy:
E. coli is a gram-negative motile rod. A few strains are non-motile (formerly referred to as Alkalescens dispar group). Some E. coli strains are capsulated.
Culture:
Specimen is inoculated on MacConkey agar and blood agar plates and incubated at 37°C for overnight.
Colonies:
The colonies are 1-4 mm in diameter, pink, circular, convex, smooth and usually non- viscous in MacConkey agar (Fig. 7.8).
Blood agar:
Colonies may be haemolytic.
Growth on other media:
Most strains do not grow or markedly inhibited in xylose-lysine-deoxycholate (XLD), DCA and SS agar.
Gram-stain:
Gram-negative bacilli.
Motility study:
Most strains are motile.
Biochemical reaction:
IMViC reactions with Esch. coli are: Indole positive methyl red positive, VP negative and Simmon’s citrate negative (IMViC++- –).
Serology:
The isolated organism is confirmed by agglutination test, first with polyvalent and then by individual specific O antisera. More than 164 E. coli serogroups are identified. H and K antigens of many of these serogroups have been identified.
Bacterial count in bacteriuria:
In urinary tract infection, sample of unspun midstream urine is inoculated in MacConkey’s agar and blood agar and incubated for overnight at 37°C. An estimate of the number of organism per ml of unspun urine sample is made by counting the number of colonies formed.
The loop of an inoculation wire is made such that a loopful amount of sample equals a volume of 0.01 ml. As each bacterial colony represents progeny of a single bacterium, the colony count in the plate when multiplied by 100 gives the bacterial count per ml sample. When bacterial count is 105 (100,000) or more per ml of urine in untreated cases of UTI, it is called significant bacteriuria.
When bacterial count is between 10,000 to 100,000 per ml, the culture may be repeated. Counts of 10,000 or less per ml are due to contamination during voiding and are insignificant. However, bacterial count in UTI may be lower than 100,000 per ml. in certain conditions, e.g. when the patient is on antibiotic therapy and in coccal infections (S. aureus, S. faecalis).
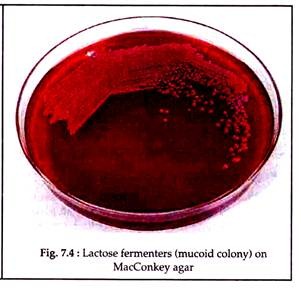
Klebsiella:
It is a non-motile, capsulated gram-negative rod and produces mucoid colony in solid media.
Habitat:
They are widely distributed in nature occurring both as commensals in human and animal mouth, upper respiratory tract and intestine, as well as saprophytes in soil, water and vegetation.
Classification:
Biochemically and antigenically, Klebsiella is classified as:
1. K. pneumoniae — also called K. aero genes.
2. K. rhinoscleromatis.
3. K. ozaenae.
Pathogenicity:
(a) K. pneumoniae:
1. Urinary tract infection, particularly those that are hospital acquired.
2. Respiratory tract infection: Occasionally it causes pneumonia.
3. Septicaemia.
4. Meningitis (especially in neonates).
5. Rarely abscesses, endocarditis, peritonitis and other lesions.
(b) K. rhinoscleromatis:
It causes rhinoscleroma, a chronic granulomatous growth of nose and pharynx.
(c) K. ozaenae:
It causes ozena in nasal mucosa, a disease characterised by foul-smelling nasal discharge with progressive atrophy of mucosal membranes.
Laboratory diagnosis:
Specimens:
Urine, sputum, pus and infected tissue depending upon site of lesion.
Microscopy:
Gram-negative, non-motile, capsulated rods.
Culture:
Large and usually mucoid colonies (due to production of extracellular slime) on MacConkey agar and blood agar. Majority of the stains produce pink colonies and MacConkey’s medium due to lactose fermentation.
Biochemical reaction:
Lactose fermenter, indole negative and citrate positive (see Escherichia coli). IMViC reactions are IMViC– – + +. Majority of Klebsiella strains are urease- producers but much slower and less intense in this regard than the Proteus strains.
Serology:
More than 80 capsular types have been identified. Identification by Quelling reaction is recommended.
Urinary tract infection:
Causative agents:
1. E. coli
2. Klebsiella spp.
3. Proteus spp, especially P. mirabilis.
4. Enterococcus.
5. Occasionally Enterobacter, Citrobacter, Ps. aeruginosa and Serratia.
6. Staph, aureus.
7. Staph, epidermidis.
Significant bacteriuria:
When bacterial count is 105 (100,000) or more per ml of unspun urine sample in untreated cases of UTI, it is called significant bacteriuria.
A standard calibrated loop of 3 mm internal diameter that can hold 1/300 ml urine is used for transferring undiluted urine sample for inoculation into MacConkey agar and blood agar and then the plates are incubated overnight.
Bacterial count:
II. Non-Lactose Fermenters:
a. Salmonella:
Habitat:
Most salmonellae are found in the gut of animals especially of pigs, cows, goats, sheep’s, rodents, hens, ducks and other poultry. They are pathogenic for their hosts and also cause disease in man. S. typhi and S. paratyphi differ from other salmonellae, in that man is the only natural host.
Classification:
Salmonellae produce 3 main types of lesions but mixed forms are common.
(a) Enteric fevers:
1. Typhoid fever — S. typhi.
2. Paratyphoid fever — S. paratyphi A, B and C.
(b) Food poisoning (gastroenteritis):
1. S. typhimurium.
2. S. enteritidis phase type 4.
3. S. dublin.
(c) Septicaemia with or without local suppurative lesion:
1. S. choleraesuis.
2. S. dublin.
3. S. virchow.
1. Typhoid fever:
(a) Incubation stage:
S. typhi is ingested with contaminated food and water. The organisms then pass from small intestine into blood (transient bacteremia) via mesenteric lymph nodes and thoracic duct. Blood stream is rapidly cleared by mononuclear phagocytic system in the liver, spleen and gallbladder.
(b) Symptomatic stage:
From the gallbladder the organisms invade the Peyer’s patches of intestine causing inflammation and ulceration. The bacilli then pass into blood leading to bacteraemia and generalized infection. Organisms are excreted in faeces and urine in third and fourth week.
2. Paratyphoid fever:
Clinically, the disease is generally milder than typhoid fever with shorter duration and incubation. S. paratyphi A and C infections are more common in tropical countries.
S. paratyphi C: It mainly causes septicaemia and important lesions caused by the organism include formation of abscess, arthritis and inflammation of gallbladder.
3. Food poisoning (enterocolitis):
Salmonella food-poisoning is caused by ingestion of contaminated food like meat, egg and milk with S. typhimurium and S. enteritidis. Symptoms occur within 10-30 hours. Food-poisoning strains can also cause septicaemia, inflammation of gallbladder and osteitis. Salmonellae causing septicaemia occasionally cause localised pyogenic lesions, such as, osteomyelitis, meningitis and deep abscesses.
Laboratory diagnosis:
Culture and isolation of salmonellae are essential to confirm a diagnosis. Identification of the isolate is based on biochemical characteristics and serology. The optimal specimen for culture varies with presentation.
(a) In a classic case of salmonella gastroenteritis faecal sample is best. Patients’ vomitus and suspected foodstuffs are also useful.
(b) In a suspected case of enteric fever, blood culture or bone marrow aspirate is most likely to yield positive results. Later, with intestinal and renal involvement, culture of faeces and urine is indicated.
The specimens to be tested at different stages of enteric fever and the percentage of positivity are shown in Fig. 7.9 and Table 7.11. General blood picture in enteric fever may show leucopenia (leucocyte count, 2,000-2,500 cumm) with relative lymphocytosis.
Isolation of the organism:
1. Culture:
Specimens of blood or bone marrow in enteric fever; faeces, vomitus or suspected food in gastroenteritis should be collected before starting treatment. As there is transient bacteraemia, there are small number of organisms in blood. Repeated culture with larger volume (5-10 ml) of blood is necessary. Blood culture is positive in 80-90% patients in first week and up to 10 days of fever.
The chances of positive culture progressively diminishes with increase in duration of illness (Fig. 7.9). Blood culture also yields positive result during relapses. Bone- marrow material culture is as reliable as blood culture and it yields positive result in 1 to 2 days after commencement of chloramphenicol therapy.
A volume of 5 to 10 ml blood collected aseptically by venepuncture is transferred directly into a blood culture bottle containing 50 to 100 ml 0.5% glucose broth or 0.5% bile broth. Although blood culture in bile broth (selective medium for salmonellae) is most ideal for salmonellae, but in practice most laboratories use glucose broth for blood culture because all microorganisms including salmonellae grow in the medium.
Larger volume of media helps in dilution of the antibacterial substances present in the blood Liquid (sodium polyanethol sulphonate) may be added in the media which counteracts the bactericidal action of blood.
Alternatively, 5 ml venous blood, collected aseptically, is allowed to clot in a sterile screw- capped universal container. After removing serum, 15 ml bile salt streptokinase broth streptokinase, 100 units per ml) is added aseptically to each bottle.
The streptokinase digests the clot causing its lysis and thereby the bacteria are released from the clot. The separated serum is utilised for Widal test. Clot culture offers a higher rate of isolation than blood culture as the bactericidal activity of serum is obviated in the technique.
After incubation overnight at 37°C , sub-culturing is done on MacConkey agar or DCA. Sub-culturing is economically carried out by spreading a loopful of broth over a sector of solid media, one-fourth of an 8.5 cm Petri dish and incubated for 24-48 hours. Colourless colonies (NLF) appear. Cultures may be discarded as negative after 10 days.
As growth may be delayed and also to eliminate the risk of introducing contamination during repeated subcultures, Castaneda’s method of blood culture may be adopted, which provides both liquid (liver infusion broth) and solid media (3% nutrient agar slope) in one bottle. It is a diphasic medium, the broth has an agar slant on one side.
2. Stool and urine culture:
Culture of faeces and urine are always positive during 3rd and 4th week of enteric fever. Repeated cultures are required for positive result. Stool culture is mainly done for detecting the carriers.
3. Duodenal juice or bile culture:
Bile is cultured to detect chronic carriers in whom the organisms are present in the biliary tract.
Identification:
In MacConkey’s agar or DCA, salmonellae grow as non-lactose fermenters which are further studied by Gram’s staining, motility preparation and biochemical reactions in different sugar media. Subculture from the colonies is made in nutrient agar to be utilised for agglutination test.
Slide agglutination test:
A loopful of isolated organism (unknown culture) from the colony in agar is emulsified in a drop of saline on a microscopic slide without spreading the drop. The emulsion must be absolutely smooth and of medium opacity. One small loopful of specific antiserum is added and then mixed by tilting the slide.
In the same way, a control of bacterial suspension in normal saline is prepared on another slide and to which no specific serum is added. Clumping of bacteria in test slide occurs within a few minutes if the antigen-antibody reaction is specific. Control saline emulsion of bacteria does not show any change.
Biochemically positive strains (Box 3) are first tested with polyvalent O serum, which reacts with salmonella strains in groups A to G, provided agglutination is not blocked by Vi antigen, which can be checked by testing all negative strains using S. typhi Vi serum. Positive results with polyvalent O serum indicates a Salmonella strain.
In the next step, the strain is tested with sera prepared against O antigens of the individual salmonella groups. The following are the most useful sera which react with factor 2, Group A factors 4 and 5, group B; with 6 and 7, group C1; with 8, group C2; with 9, group D; and with 3, 10, 15 and 19, group E.
When the strain is positive with individual salmonella O serum, and biochemically it is typically S. typhi, the strain is tested against S. typhi O serum, factor 9. Prompt agglutination indicates that the microorganism belongs to Salmonella group D. Its identity is established as S. typhi by agglutination with salmonella H specific serum which reacts with flagellar antigen d.
In a non-typhoid salmonella, the strain is tested for agglutination with O and H sera for groups A, B and C. When unusual serotypes are encountered, the same should be referred to the National Salmonella Reference Centre (Central Research Institute, Kasauli, for human strain, and Indian Veterinary Research Institute, Izatnagar, for salmonella of animal origin).
Subtyping:
Subtyping methods are frequently used for the common serotypes (S. typhi, S. typhi- murium and S. enteritidis) which include phage typing, bio-typing, and more recently introduced genotyping methods (plasmid finger printing). These techniques are employed in CDC for subtyping within serotypes of Salmonella.
Serological test:
1. Widal test:
It is an agglutination test which detects presence of serum agglutinins (H and O) in patient’s serum with typhoid and paratyphoid fever. Salmonella antibody starts appearing in serum at the end of first week and rises sharply during the 3rd week of enteric fever.
It is preferable to test two specimens of sera at an interval of 7 to 10 days to demonstrate a rising antibody titre. Convalescent sera from salmonella gastroenteritis cases often agglutinate a suspension of the causal serotype which helps in retrospective diagnosis.
Procedure:
In Widal test, two types of tubes were originally used: (i) Dreyer’s tube (narrow tube with conical bottom) for H agglutination, and (ii) Felix tube (short round-bottomed tube) for O agglutination. Nowadays 3 x 0.5 ml Kahn tubes are used for both types of agglutination.
A serial two fold dilution of patient’s serum in normal saline (1: 20, 1: 40 and so on up to 1,280 or more) is prepared in 8 small (3 x 0.5 ml) test tubes for each series; 7 for serum dilutions and 8th for a non-serum control.
To the diluted serum and control saline equal volume (0.4 cc) of antigen suspensions (TH, TO, AH and BH) are added and mixed thoroughly by shaking the rack and then the mixtures are incubated at 37°C for 4 hours and read after overnight refrigeration at 4°C. Some workers recommended incubation in a water bath at 37°C overnight.
Observation:
Loose and cotton-woolly clumps are formed in H agglutination and a disc-like granular deposit in O agglutination at the bottom of tube. Control tube shows a compact deposit. The Maximum dilution of serum at which agglutination occurs indicate the titre of antibodies.
The routinely used antigens are H and O of S. typhi, H of S. paratyphi A and B. As paratyphoid O antigen cross reacts with typhoid O antigen due to the sharing of factor 12 by them, paratyphoid O antigens are not used.
Preparation of Widal antigen:
H suspension of bacteria is prepared by adding 0.1% formalin to a 24 hours broth culture or saline suspension of an agar culture. For preparation of O suspension of bacteria, the organisms are cultured on phenol agar (1: 800). Standard smooth strains of the organism are used; S. typhi 901, O and H strains are employed for this purpose.
Interpretation of Widal test:
1. Agglutinin starts appearing in serum by the end of 1st week with sharp rise in 2nd and 3rd weeks and the titre remains steady till the 4th week after which it declines.
2. Rising titre:
Demonstration of rising titre of four-fold or greater of both H and O agglutinins at an interval of 4 to 7 days is the most important diagnostic criterion.
3. In a single test, a titre of 100 of O or more and a titre of 200 of H agglutinins signifies presence of active infection, but that has to be interpreted taking into consideration the following factors:
(i) Local titre:
Due to sub-clinical infection of salmonellosis in endemic area, low titre of agglutinins is present in the serum of normal individuals, which may cause positive reaction. This is known as local titre. Local titre is up to 80 in Kolkata and 60 in Siliguri.
(ii) Immunisation:
In immunization with TAB vaccine, vaccinated individuals may show high titres of antibody (H antibody titre 160 or more) to each of the salmonellae.
(iii) Anamnestic reaction:
Persons who had past enteric infection or who have been vaccinated may develop transient fever like malaria, influenza etc.
(iv) Non-specific antigens (e.g. fimbrial antigen) may produce false positive result.
(v) Antibiotic treatment:
When treatment with chloramphenicol is started before the appearance of agglutinins, they are unlikely to appear subsequently; if the antibody is already present, no further rise in titre is expected.
(vi) Carriers:
Widal tests may be negative in many healthy carriers and some have to be detected by Vi agglutination test.
2. Other serological tests:
ELISA is sensitive method of measuring antibody against the lipopolysaccharide of Salmonellae, titre of IgM antibody corresponds fairly well with the Widal O titre. ELISA in vertical flow membrane format (Typhi- DOT) detects Vi Ag in blood/serum at an early stage of the disease.
b. Shigella:
Habitat:
Shigella species are exclusively parasites of human and other primates and cause bacillary dysentery in man.
Classification:
Shigellae are gram-negative non- motile bacilli. Antigenically, shigellae are divided into four groups (A, B, C, D) based on specificity of O antigen. These groups are differentiated by a combination of biochemical reactions and antigenic structure. Mannitol fermentation reactions are important, group A is mannitol negative and the rest are mannitol positive.
Pathogenesis:
Shigella species cause bacillary dysentery (shigellosis). Infection is transmitted by faecal-oral route. S. dysenteriae type 1 (S. shiga) produces exotoxins that causes most severe form of disease. S. flexneri and S. boydii cause less severe dysentery and are prevalent in tropical countries including India. S. sonnei is the cause of most dysentery in Britain.
The organisms are taken up by the epithelial cells of distal parts of the colon with necrosis of surface epithelial cells leading to an acute inflammation in lamina propria and sub-mucosa. Necrotic epithelia sloughs forming superficial ulcers which leads to bleeding mucosa.
Laboratory diagnosis:
To confirm diagnosis, shigella must be isolated in pure culture from an adequate sample. Specimens include fresh stool, mucous flakes, and rectal swabs.
A. Microscopical examination of stool:
Cover slip preparation in saline and iodine shows large number of pus cells (neutrophils) with degenerated nuclei, RBC, and macrophages. The presence of protozoa, cysts or helminthic ova is excluded. The normal bacterial flora is considerably diminished. Fluorescent antibody technique is of some help in rapid diagnosis of a case but it is not usually practiced.
B. Bacteriological examination:
I. Culture:
Media:
MacConkey’s agar, DCA, S-S agar, Selenite F broth.
A loopful of material is inoculated on selective media like MacConkey’s agar or SS agar media.
Selenite-F broth (0.4%) is used as enrichment and transport medium which permits rapid growth of enteric pathogens while temporarily (for 9-12 hours) inhibiting the growth of E. coli. Organisms from selenite-F broth are sub-cultured in MacConkey’s agar after 24 hours incubation at 37°C.
Colourless colonies appear on MacConkey’s agar medium after 12 to 18 hours incubation which is further tested by smear examination, motility preparation and biochemical reactions. Shigellae are Gram-negative non-motile bacilli.
II. Biochemical reactions:
Urease, citrate, H2S and KCN negative; indole and M R positive Gram-negative non-sporing bacillus is suggestive of a shigella strain (Fig. 7.10). S. sonnei is a late lactose fermenter.
III. Slide agglutination test:
It is done by using polyvalent antisera of three groups (A, B and C) of shigella and antiserum of group D (S. sonnei), one by one against the isolate. Monovalent antisera are used for the group for which agglutination has occurred with polyvalent antisera. Then type specific antisera for strains belonging to Group A, B or C is used for agglutination test.
Occasionally, agglutination may not occur due to masking of O antigen by K antigen, which can be removed by boiling the bacterial suspension at 100°C for 60 minutes.
IV. Colicin typing:
It is done for group D strains.
V. Sereny test may be done to confirm the invasiveness of the isolated strain of shigella, although, it is seldom practiced.