Here is a list of fourteen major diseases that are caused by bacteria: 1. Tetanus 2. Anthrax 3. Tuberculosis 4. Diphtheria 5. Meningitis 6. Pertussis 7. Streptococcal Pneumonia 8. Gonorrhea 9. Syphilis 10. Leprosy 11. Cholera 12. Botulism 13. Shigellosis 14. Typhoid Fever.
Contents
- Disease # 1. Tetanus:
- Disease # 2. Anthrax:
- Disease # 3. Tuberculosis:
- Disease # 4. Diphtheria:
- Disease # 5. Meningitis:
- Disease # 6. Pertussis:
- Disease # 7. Streptococcal Pneumonia:
- Disease # 8. Gonorrhea:
- Disease # 9. Syphilis:
- Disease # 10. Leprosy:
- Disease # 11. Cholera:
- Disease # 12. Botulism:
- Disease # 13. Shigellosis (or Bacillary Dysentery):
- Disease # 14. Typhoid Fever:
Disease # 1. Tetanus:
Tetanus (Greek tetanos means to stretch) is caused by Clostridium tetani. C. tetani is a Gram- positive, anaerobic and spore forming bacterium, the endospores of which are found in soil, dust and faeces of many farm animals and humans.
However, bacterium can exists in air, water and human intestine. Moreover, it can survive in dead anaerobic matter because the bacterium is basically a saprobe rather than a parasite. In India incidence of tetanus is high.
Transmission of the bacterium takes place through skin wound. The endospores enter in wounds/breaks caused in skin. These germinate if oxygen tension is low. However, the bacteria living in intestine do not cause disease. These are discharged through faeces.
In the wound the neurotoxin, tetanospasmin, is released after the death and break down of bacteria. Tetanospasmin is an endopeptidase that breaks the synaptic vesicle membrane protein, synaptobrevin. This in turn inhibits exocytosis and release inhibitory neurotransmitters at synapses within the motor nerves of spinal cord. This results in stimulation of skeletal muscles that lose its control.
Tetanospasmin causes tension and twisting in skeletal muscles present around the wound. The jaw muscles become tight. Consequently, there develops trismus (“lock jaw”) which is an inability to open the mouth due to spasm or contraction of master muscles.
In severe contraction of muscles opisthotonos takes place. It is a situation when back bows backwardly, and back and heels approaches each other to form an arch. Due to contraction of diaphragm and intercostal respiratory muscles deaths occur.
Immunization and Control Measures:
Tetanus is prevented by using tetanus toxoid. The tetanus toxoid is a formaldehyde-treated toxin that is precipitated in the form of salt of aluminum to increase its immunizing potency. The tetanus toxoid is given with DPT programmes. After a few months of birth, initial dose is given.
The second dose should be given after 4-6 months of the first dose. Finally, the reinforcing dose should be given 6 to 12 months after the second dose. Between the age of 4 to 6 years, a final booster is given. A single booster dose can provide protection for 10 to 20 years.
One to too many doses over a period of years results in hypersensitivity reactions. Therefore, when an individual has a wound infection, he should be given booster doses.
The tetanus cannot be controlled because of survival of bacterium in soil for a long duration. Treatment of tetanus is not very effective. About 30-90% cases become fatal. Hence, preventive measures must be adopted by active immunization with toxoid, prophylactic use of antitoxin, and using penicillin.
Disease # 2. Anthrax:
Anthrax (Greek anthrax means coal) is caused by Gram-positive, Bacillus anthracis. It is highly infectious disease that spread through contact of infected animals (goat, sheep, and catties) with humans having abrasion or cut on skin. Consequently, the endospores come in the contact of cuts, infect skin and develop (between 1-15 days) cutaneous anthrax.
In addition, when endospores are inhaled, they result in pulmonary anthrax; similarly, when endospores are ingested, they cause gastrointestinal anthrax. However, endospores can remain viable in soil for a long duration.
It infects skin, wounds and ulcerate the skin. Pulmonary anthrax is similar to influenza. The disease becomes fatal when the bacteria infect blood stream. The bacteria secrete anthrax toxin (a complex exotoxin system composed of three proteins). The toxin develops symptoms that include headache, fever, and nausea.
The disease is diagnosed directly through identifying the bacteria, culture of bacteria and serologically. The control measures are vaccination of catties, animals, and humans handling them. The antibiotics recommended for patients are penicillin G, or penicillin G plus streptomycm. The other soil-borne bacterial diseases are given in Table 25.3.
Disease # 3. Tuberculosis:
For the first time Robert Koch identified Mycobacterium tuberculosis as the causal agent of TB (tuberculosis). During that period TB caused 1/7 of death in Europe. At present TB is the global health problem. About 20% of the world’s population is suffering from TB and about 8 million people are victimized each year. Approximate annual death is 3 million.
Commonly tuberculosis occurs among the homeless, malnourished persons or alcoholic drinkers. This bacterium spreads through droplet nuclei and the respiratory route. Bovine tuberculosis is caused by M. bovis in cows and catties. It is equally dangerous. M. bovis spreads to humans through contaminated milk.
Mycobacterium is rod-shaped and acid fast (stained with acid fast technique by Ziehl- Neelsen Carbol-fuchsin stain). Therefore, the cells take red stain. The bacterium infects the respiratory tract and established in lung tissues. After being phagocytosed by macrophages the bacteria are enclosed into the small and hard tubercles which are the characteristic feature of the disease. Hence it gives the name of disease as tuberculosis.
In X-rays tubercles can be observed. The symptoms include cough, pain in chest, fever and secretion called sputum. The sputum appears red or rust coloured if mixed with blood in lung cavity.
Bacteria remain alive in macrophages. Sometimes the tubercle lesions liquefy and form air-filled cavities where from bacteria can spread new foci of infections throughout the body.
This spreading is called miliary tuberculosis due to development of millet seed like many tubercles:
(i) Immunity:
Against infection by M. tuberculosis patients develops a cell mediated immunity which involves the sensitized T cells. It is the basis of tuberculin skin test. In this test a purified protein derivative of M. tuberculosis is injected into the patients (Mantoux test).
If the pathogen is present in body of patient, sensitized T cells react with these proteins. Thereafter, a hypersensitivity reaction occurs within 48 hours. Consequently around the injected site there appears hardening and reddening area.
(ii) Diagnosis of Tuberculosis:
Laboratory diagnosis of tuberculosis includes isolation of the acid-fast bacterium, chest X-ray by commercially available DNA probe, HPLC test, and the Mantoux or tuberculin skin test. Chemotherapy is done by administering isoniazid plus rifampin, ethambutol and pyrazinamide. These are administered simultaneously for 12 to 24 months. BCG (Bacillus-Calmette-Guerine) vaccine is used for treatment of tuberculosis.
Disease # 4. Diphtheria:
Diphtheria (Greek diphthera means membrane, and ia means conditions) is a serious airborne contagious disease. It is caused by Corynebacterium diphtheriae which is a Gram-positive bacterium. Like tuberculosis, diphtheria also occurs in poor people living in crowded condition.
C.diphtheriae is club-shaped and contains many metachromatic granules in cytoplasm. It is associated with leathery membrane. In India, it has a major problem. It is inhaled through droplets and reaches to respiratory tract and infects it. Typical symptoms of diphtheria include a thick mucopurulent (containing mucus and pus) nasal discharge, vomiting, headache, fever, cough and stiffness in the neck and back.
The bacteria produces diphtheria toxin which is an exotoxin that causes an inflammation and greyish pseudo-membrane on respiratory mucosa. The exotoxin is absorbed by the body into the circulatory system and transported throughout the body.
Hence, it may destroy kidney, nervous tissues and even heart by producing toxic proteins which is called diphtheria toxin. Diphtheria is diagnosed by culturing the bacterium and observation of pseudo-membrane in throat. To neutralize the effect of endotoxin, generally antitoxin is given. Penicillin and erythromycin are prescribed for the treatment of infection.
Sometimes cutaneous diphtheria also develops when C. diphtheriae infects skin, skin lesions or wounds causing slow healing ulceration. This disease occurs when people of over 30 year’s age have a weakened immunity, particularly living in tropical regions. Worldwide immunization programme is being launched with the DPT (diphtheria-pertussis-tetanus) vaccine.
Disease # 5. Meningitis:
Meningitis (Greek meninx means membrane and itis means inflammation) is an inflammation of meninges (membranes) of brain or spinal cord. This disease is caused by bacteria, fungi or viruses and, therefore, divided into two: bacterial meningitis or septic meningitis and the aseptic meningitis syndrome (Table 25.1).
Due to a large number of causes of meningitis, accurate identification of causative agents must be done before the treatment of disease. The respiratory secretion of carriers acts as a source of meningitis. The bacteria colonize the nasopharynx and cross the mucosal barrier. Thereafter, these enter the blood stream and cerebrospinal fluid. Consequently, they cause inflammation of the meninges.
Specific antibiotics such as penicillin, chloramphenicol, cefotaxime, ofloxine, etc. are used for the treatment of meningitis. Moreover, vaccines against S. pneumoniae and N. meningitis are also available for treatment.
Disease # 6. Pertussis:
Pertussis (Latin per means intensive, and tussis means cough) is also known as whooping cough. This disease is caused by a Gram-negative bacterium, Bordetella pertussis. It is highly contagious disease and affects the children first. About 95% population of the world is affected by whooping cough, and about 5,00,000 patients die each year.
The causal agent was first isolated by Jules Bordet and O. Gengau in 1906. It is a small, fragile, and Gram-negative rod. The bacterium is transmitted through droplets of infected persons and enters into the healthy one after inhalation. It is established from 7 to 14 days of infection.
The bacterium is attached to the ciliated epithelial cells of upper respiratory tract. It produces an adherence factor called filamentous haemagglutinin that recognises complementary molecule of the host cell.
After being attached to the epithelium, the bacterium produces several toxins. These toxins develop the symptoms. The most important toxin is pertussis toxin. In its presence the tissues become susceptible to histamine and serotonin, and response of lymphocyte is increased.
In addition, B. pertussis also produces an extracellular enzyme (adenylate cyclase) and a tracheal cytotoxin and a dermonecrotic toxin. These destroy the tissue of epithelium. Due to secretion of thick mucus the ciliary action is impeded and the ciliated epithelial cells die.
Laboratory diagnosis of this bacterium includes: culture of the bacterium, fluorescent antibody, staining of smears from nasopharyngeal swabs and serological tests. The chemotherapeutic agents are chloramphenicol, tetracycline or erythromycin. The children of 2-3 years age are recommended for vaccination with DPT vaccine.
Disease # 7. Streptococcal Pneumonia:
Streptococcal pneumonia is caused by the bacterium. Streptococcus pneumoniae (syn. Diplococcus pneumoniae) which is an inhabitant of normal microflora of nose. Therefore, streptococcal pneumonia is considered an endogenous infection. S. pneumoniae is a Gram-positive bacterium containing a capsule of polysaccharide. The capsule provides virulence to
the bacterium because of inability of binding of antibodies to the bacterium. Pneumonia is caused by the bacterium present in respiratory tract. Move over, about 60 to 80% of all respiratory diseases known so far is caused by this bacterium. Pneumonia generally develops in those persons who already have viral infection of the respiratory tract, physical injury of tract, diabetes or alcoholism.
S. pneumoniae multiplies rapidly in alveolar spaces of lung. The alveoli are filled with blood and fluid which finally become inflammed. That is why after coughing red-coloured sputum comes out from the lung. When entire lobes of lung are infected, it is known as lobar pneumonia.
When both sides are infected, it is called double pneumonia. However, if the branchial tree is infected showing scattered patches, it is called bronchopneumonia. The symptoms of pneumonia are chilling, breathing with difficulty and chest pain. Pneumonia is diagnosed by X-ray, culture of the bacterium and biochemical test.
Presence of capsule around the cell wall provides virulence to the pathogen. This also inhibits the binding of antibodies to the cell; thus it inhibits phagocytosis. The antibiotics recommended for the treatment of pneumonia are penicillin G, cephotaxime, ofloxacin and ceftriaxone.
The persons, sensitive to penicillin, can take erythromycin or tetracycline. For debihtated persons a pneumococcal vaccine (Pneumovax) is also available.
There are several bacterial diseases in human which are transmitted sexually or through contact (Table 25.4).
Disease # 8. Gonorrhea:
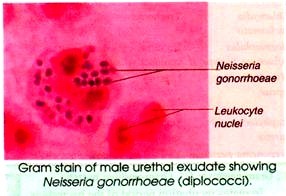
Gonorrhea (Greek gono means semen, and rhein means to flow) is caused by Neisseria gonorrhoeae which is named after Albert L.S. Neisser who cultured the bacterium first in 1879. It is small Gram- negative, oxidase-positive, diplococcus bacterium. The bacteria are also referred to as gonococci. Gonorrhea is a sexually transmitted disease of the mucus membrane of genito-urinary tract, eyes, rectum and throat.
Transmission of bacteria occurs during intercourse. Bacteria adhere to microvilli of mucosal cells by pili and protein II that function as adhesion. Due to attachment bacteria are not washed away by normal vaginal discharge or by strong flow of urine. In female, the bacterium infects the epithelial cells of urethra and cervix.
It takes about 7-21 days to develop symptoms. These occur in some vaginal discharge. In severe cases, passage of fallopian tube is blocked by pus and scar tissues resulting in sterility. Female feels pain and burning sensation while urinating. Normal menstruation cycle in the patient is interrupted.
Gonococci disseminate most often during menstruation, a time in which there is increased concentration of free irons available to the bacteria. In both the sexes gonococcal infection may occur leading to gonorrheal arthritis, gonorrheal endocarditis, or gonorrheal pharyngitis.
As the newborns pass through an infected birth canal, gonorrheal eye infection occurs in them. This disease is called ophthalmia neonatorum or conjunctivitis of the newborns’. However, about 50% of infected females transmit this disease unknowingly.
In males incubation period of the bacteria is 2 to 8 days. Primary infection occurs in urethra. The symptoms include a thin and watery discharge followed by white to creamy pus from penis. The males feel frequent painful urination with burning sensation.
The flow of sperms is blocked when epididymis is infected. This leads to sterility. Symptoms in male are more serious than that in female. The bacteria also infect eyes after being transmitted through fingertip, towel, etc. and cause corneal infection which is known as keratitis.
Diagnosis of N. gonorrheae in laboratory is done based on oxidase-reaction, Gram-stain reaction and colony and cell morphology. Performance of confirmation test is also necessary.
Effective methods for control of this sexually transmitted disease are public education, diagnosis and treatment of asymptomatic patients, use of condom and quick treatment of infected individuals. About 60% of this disease occurs in individuals of 15-24 years age.
The recommended antibiotics for treatment of gonorrhea are:
(i) Penicillin G plus probenecid,
(ii) Ampicillin plus probenecid,
(iii) Ceftriaxone or ofloxacin plus doxycycline for 7 days, or
(iv) Streptomycin. To prevent conjunctivitis of the newborns, tetracycline, erythromycin, povidone-iodine, or silver nitrate in dilute solution is placed in the eyes of newborns. Penicillin-resistant strains in 1980 and tetracyline-resistant strains in 1980 have been reported.
Disease # 9. Syphilis:
Venereal syphilis (Greek syn means together, and philein means to love) is a contagious sexually transmitted disease caused by a spirochete, Treponema pallidum. Congenital syphilis is a disease which is acquired in uterus from the mother.
During the end of 15th century, syphilis was recognized in Europe. According to one hypothesis syphihs is of New World Origin. Christopher Columbus (1451-1506) and his crew acquired it in West Indies and introduced into Spain when returned from their historic voyage. The other hypothesis holds that syphilis has been endemic for centuries in Africa where from it was transported to Europe through the migrants during 1500.
In 1530 Girolamo Fracastoro, a poet and physician of Italy, has written about syphilis as a disease transmission of “seeds” which took place through sexual contact. In 18th century venereal transmission of syphilis was shown. The term venereal is derived from Venus, the Roman Goddess of love.
In 1838, P. Ricord demonstrated the various stages of syphihs. In 1905 Fritz Schaudinn and Erich Hoffmann discovered the causitive bacterium. In 1906 August Von Wassermann introduced the diagnostic test that bears his name. In 1909, P. Ehrich applied the therapy of syphilis by using arsenic derivative, arsephenamine or salvarsan.
T. pallidum moves by axial filament and enters the body through mucus membrane or abrasion or wound or hair follicle on the skin. Sexual intercourse is the most common way of transmission and contact of the bacteria. However, there is 10% chance of acquiring bacteria from single expose to an infected sex partner.
In untreated adults the disease occurs in the following three stages:
(i) Primary Syphilis:
In the primary stage incubation period is of about 10 days to 3 weeks. This stage is characterized by a small painless and reddened ulcer or chancre (French canker a descructive sore). Chancre has a hard ridge that looks as the infection site and consists of spirochetes.
Disease is transmitted if contact with chancre is made during sexual intercourse. About in 30% cases chancre disappears and disease does not spread further. In others the spirochetes are distributed throughout the body via blood streams.
(ii) Secondary Syphilis:
The second stage is established within 2 to 10 weeks after the primary lesions. This stage is characterized by a skin rash. At this stage about 100% cases are serologically positive. At this stage symptoms include loss of patches of hairs, malaise and fever. There are flat warts like lesions which are filled with spirochetes.
(iii) Tertiary Syphilis:
After several weeks the disease becomes latent. During latent period disease is not infectious except transmission from mother to foetus. This is called congenital syphilis. After several years (more than a decade) a tertiary stage develops in approximately 40% of cases when secondary syphilis remains untreated.
The symptoms of tertiary syphilis include formation of degenerative lesions (gummas) in the skin, bone, cardiovascular and nervous systems. At this stage number of spirochetes is drastically reduced. This results in mental retardness, blindness, a “shuffle” walk leading to paralysis. Several famous persons such as Henery VIII, Adolf Hitler, Oscar Wilde, etc. have been sufferer of syphilis.
Syphilis is diagnosed through clinical history, thorough physical examination, immunofluorescence examination of fluid from lesions to observe typical mortality.
The serological tests include:
(i) Test for non-treponemal antigen by VDRL (Venereal Disease Laboratories test), RPR (Rapid Plasma Reagin test). Complement fixation test or the Wassermann test, and
(ii) Test for treponemal antibodies (FTA-ABS, fluorescent treponemal antibody-adsorption test; TPI, T. pallidum immunization; T. pallidum complement fixation; TPHA, T. pallidum haemagglutination).
Preventive and control measures of syphilis are:
(i) Public education,
(ii) Prompt treatment of new cases,
(iii) Treatment of source of infection and contact,
(iv) Maintaining sexual hygiene, and
(v) Prophylaxis (condoms).
The highest incidence of syphilis is in the age group between 20 and 39 years.
Disease # 10. Leprosy:
Leprosy (Greek Leprosei means scaly, scabby, rough) or Hansen’s disease is caused by Mycobacterium leprae. This bacterium was first observed in 1874 by Gerhard Hansen, a Norwegian physician. So far the bacterium could not be cultured on artificial medium. M. leprae is acid-fast rod, slow grower and heat-sensitive bacterium.
Leprosy is a contact disease that degenerates the tissues and deforms the body organs. Humans are the only reservoir of the disease. According to WHO report, there are about 10 millions of cases especially in South Asia, Africa and America.
Disease is transmitted to children when prolonged exposures to infected persons are made. For family contact nasal secretions are the infectious materials. It takes about 3 to 5 years to establish properly. The bacterium infects peripheral nerves and skin cells and enters intracellularly.
The earliest symptoms of leprosy are slightly pigmented eruptions of skin which are several centimeter in diameter. In early stage about 75% individuals heal the lesions due to development of cell-mediated immunity. In 25% leprosy develops due to weak immune response. There are two forms of leprosy.
(i) Tuberculoid (Neural) Leprosy:
Tuberculoid leprosy is mild, non-progressive and associated with delayed type hypersensitivity reaction to antigens on the surface of M. leprae. The nerves are damaged and regions of the skin that have lost sensation are surrounded by a border of nodules. This results in atropy of muscles and disfiguring of skin and bones, and curling of fingers. The outer ear and nasal cartilage degenerate.
(ii) Lepromatous (Progressive) Leprosy:
In the infected individuals, who do not develop hypersensitivity, there occurs progressive form of disease which is known as lepromatous leprosy. A large number of M. leprae develops in the cells of skin.
This type of leprosy is characterized by lepromas (tumour like growths) on the skin and along respiratory tract. The bacteria kill skin tissue resulting in progressive loss of facial feature, fingers, toes, etc. Disfiguring nodules form all over the body. The nerves are less damaged as compared to tuberculoid leprosy.
Since the bacterium cannot be cultured in vitro, it can be diagnosed by acid-fast staining, and serologically such as fluorescent leprosy antibody adsorption test, DNA amplification, ELISA test. Long-term treatment with sulfone drug, dapson, and rifampicin with or without clofazimine has been recommended. Mycobacterium W vaccine is also being used.
Food and water are the essential requirements of our body. There are many bacteria that contaminate food and water, and through these they enter in our intestine. Contaminated food causes stomach and intestinal disorder that is known as food-poisoning.
The food-poisoning is caused due to secretion of exotoxin by the bacteria that contaminate food. After ingestion bacteria colonize the gastrointestinal tract, infect the tissue and secrete exotoxin. This condition is known as food intoxication because only the toxin is ingested and living bacteria are not required.
The enterotoxin poisoning produces the symptoms: nausea, vomiting and diarrhoea. Worldwide death by diarrhea is second to respiratory disease. Diarrhoea occurs maximum in children causing 5 million deaths in Asia alone.
A summary of food borne diseases is given in Table 25.2. Some of the food- and water-borne diseases are discussed in this section:
Disease # 11. Cholera:
Since the time immemorial cholera (Latin Chole means bile) has caused pandemics in Asia, and Africa. It is caused by a Gram-negative, slightly curved bacterium. Vibrio cholerae, that contains a single polar flagellum (Fig. 25.1).
It was cultured for the first time in 1883 by Robert Koch. It has several serological groups such as 01, 02, 0139 and two bio- types V. cholerae and EL Tor. The mortality rate without treatment is 50%, and with care and treatment 1%.
This bacterium is acquired after taking food and water contaminated by faecal material from patients or carriers. In 1961 the El Tor biotype of V. cholerae 01 strain was the cause of cholera pandemic and in 1996 strain V.cholerae 0139 emerged in Calcutta in India. The incubation period of the bacteria is 24-72 hours. It adheres to the mucosa of small intestine and secretes a cholera toxin, choleragen. Cholera-toxin is a protein.
It possesses two functional units: an enzymatic subunit A and an intestinal receptor-binding subunit B. The sub- unit A acts as diphtheria toxin. It enters into the epithelial cells of intestine, binds to ADP – ribosyl group and activates the enzyme adenylate cyclase. Thus, choleragen induces the secretion of water and chloride ions and inhibits absorption of sodium ions.
The patients loose water and electrolyte. This results in cramping of abdominal muscles, vomiting, fever and watery diarrohea. During infection a person can lose 10-15 liters of fluid. Finally patients die due to loss of water and electrolytes and increased amount of blood proteins that leads shocks and collapse of circulatory system.
Laboratory diagnosis of the bacterium is by culture from faeces, and agglutination reaction with specific antisera. The patients are immediately rehydrated with NaCl plus sucrose solution. The antibiotics recommended to patients are tetracycline, trimethoprim, sulfamethoxazole or ciprofloxacin. Proper sanitation of water supplies must be done regularly.
Disease # 12. Botulism:
Botulism (Latin botulus means sausage) is a type of food poisoning caused by Clostridium botulinum. It is an obligately anaerobic, endospore forming. Gram-positive, rod-shaped bacterium which is commonly found in soil as well as in aquatic deposits.
The home canned food, not sufficiently heated to kill contaminated C. botulinum endospores, acts as source of infection. The endospores are ingested. They germinate and produce botulinum toxin during vegetative growth.
The toxin has effects on nervous systems, hence it is a neurotoxin. It binds to synapses of motor neurons and breaks the synaptic vesicle membrane protein, synaptobrevin. Consequently it inhibits the exocytosis and release of neurotransmitter acetylcholine. This causes failure of muscle contraction in response to activity of motor neurons leading to paralysis.
Symptoms occur within 18-24 hours of ingestion of toxin. Symptoms include blurred vision, difficulty in swallowing and speaking, muscle weakness, nausea and vomiting. About one-third patients die without treatment due to failure of respiratory or cardiac system.
In the U.S.A. about 100 cases of infant botulism are reported each year. Therefore, infant botulism is most common. Laboratory diagnosis is by inoculation of mice with patient’s blood serum, stools or vomitus to prove toxigenicity. Haemagglutination test is also done.
Prevention and control of botulism can be done by:
(i) Strictly adopting food processing practices by food industry,
(ii) Educating the people for safe preserving of homemade food materials,
(iii) Discouraging the infants of below one year age from feeding honey, and
(iv) Giving large doses of botulism antitoxin to patients.
Disease # 13. Shigellosis (or Bacillary Dysentery):
Shigellosis is a diarrhoeal illness. It results from inflammatory reaction of the intestinal tract caused by Shigella. Four species of Shigella are known to be associated with shigellosis.
Shigella is a Gram-negative, non-motile, facultative and rod-shaped bacterium which is transmitted by the four ‘Fs’ i.e. food, fingers, faeces and flies. It is most prevalent among children of 1 to 4 years age. Worldwide deaths by bacillary dysentery are around 500,000 patients per annum. In 1984 a severe outbreak of shigellosis was noticed from West Bengal.
After acquiring the bacterium, its proper establishment in intracellular space of epithelial cells of colon occurs within 1-3 days. The mucosal cells phagocytose the bacteria. Bacteria disrupt the phagosome membrane and reproduce within it.
It also secretes endotoxin and exotoxin that do not spread beyond the epithelium of colon. Consequently, a watery fluid containing blood, mucus and pus starts coming out at intervals. When the case becomes serious the colon is ulcerated.
The disease lasts an average of 4 to 7 days in adults and becomes self-limiting, whereas in infants and children it is fatal because of malnutrition, neurological disorders and failure of kidney.
Preventive and control measures are: good personal hygiene and clean water supply, and treatment with trimethoprim-sulfamethaxazole or fluoroquinolones. Development of antibiotic-resistant strains of Shigella has also been reported.
Disease # 14. Typhoid Fever:
Typhoid (Greek typhoides means smoke) fever is caused by Salmonella typhi which is a Gram-negative, rod-shaped bacterium resistant to environmental conditions. Fresh water and food act as reservoir of the bacterium. However, it spreads through contaminated water.
Typhoid Mary:
During 1900s thousands of typhoid fever cases and a few deaths were reported in the U S.A. Most of these cases arose due to drinking of contaminated water of eating foods handled by persons suffering from typhoid fever and shedding S. typhi. One of the most famous carriers of this disease was Mary Mallon.
Mary Mallon worked as cook in seven houses in New York City between 1896 and 1906. During the time of her work in these homes, 28 cases of typhoid fever occurred. The New York City Health Department arrested Mary and admitted to the hospital Mary’s stool was examined. She was found to carry typhoid fever bacteria but she did not show external symptoms of the disease.
In 1908, an article was published in the J. Amer. Med Ass as “Typhoid Mary”. After being released she pledged not to act as cook. But she changed her name and began to work as cook again.
For five years she spread typhoid by shedding bacteria. She was again arrested and held in custody for 23 years until she died in 1938. During her life time, she was linked with 10 out breaks of typhoid fever, 53 cases and 3 deaths. Thus, Mary was one of the most famous typhoid carriers.
S. typhi after ingestion/drinking of water, colonize the small intestine, penetrate the epithelium and spread to lymphoid tissues, blood, liver and gall bladder. Symptoms include fever, headache, abdominal pain and malaise. This remains as such for several weeks.
After 3 months most of the patients do not shed bacteria, whereas a few of them do for prolonged time without external symptoms. In these patients bacteria grow in gall bladder, and reach to intestine. Laboratory diagnosis is made by demonstrating the bacteria in stool, urine and blood, and also through serological test.
The preventive and control measures include:
(i) Purification of drinking water, milk pasteurization, and prevention of handling of food by carriers,
(ii) Complete isolation of the carriers,
(iii) Use of antibiotics such as ceftizoxane, trimethoprim-sulfamethoxazole or ampicillin, and
(iv) Use of vaccine for high risk individuals.