‘The antibiotics’ are secondary metabolites or biochemical secreted by microorganisms which, ‘ in low concentration, inhibit the growth or kill other microorganisms, i.e., the antibiotics are ‘antimicrobial agents of microbial origin’. Although some 6,000 antibiotics are known to exist, only about 100 are marketed. About 200 new antibiotics are discovered every year.
Microorganisms belonging to three orders viz., Eubacteriales, Actinomyces and Moniliales have contributed immensely to the rise and development of the antibiotic industry. However, out of 6 000 antibiotics, about 1,000 have been obtained from just six genera of filamentous fungi (e.g., Penicillium and Cephalosporium) and about 2,000 from just three genera of bacteria (e.g., Streptomyces, Bacillus and Micromonospora).
To be truly useful, an antibiotic must possess following qualities in it:
(i) Antibiotic should be of “broad spectrum”, i.e., it should have the ability to inhibit/kill a number of different types of pathogenic microorganisms.
(ii) It should check the development of resistant forms of pathogenic microorganisms.
(iii) It should not result in undesirable side effects in the host.
(iv) It should not disturb the “normal” microbial flora of the host. Such a disturbance may upset the balance of nature.
(1) Penicillin:
Alexander Fleming discovered penicillin secretion by the mould Penicillium notatum in 1929. While working in a hospital laboratory in London. He saw that Staphylococcus colonies were lysed due to fungal activity. However, when Chain (1939) purified the active material, called penicillin, it proved remarkably effective in certain infections. Penicillin is not a single chemical compound but a group of substances of related structure and activity.
There are six penicillins: Penicillin G (benzyl penicillin V (phenoxymethyl penicillin), penicillin F (A2 – pentenyl penicillin), penicillin X (p-hydroxybenzyl penicillin), penicillin K(n-heptyl penicillin) and penicillin O (allyl- mercaptomethyl penicillin). Penicillin is selective for Gram-positive bacteria, some spirochaetes and the Gram-negative diplococci (Neisseria).
It was World War II that provided stimulus for commercial production of penicillin; and various strains of Penicillium chrysogenum are used for the purpose. At present, almost 50 years later, such strains of the fungus are available that yield 104 times more than the original isolate. Production has also been dramatically increased by improvements in media and to fermenter design.
Phenyl ethanoic acid (phenyl acetic acid) is now routinely added to the media since this induces the synthesis of a metabolic precursor of penicillin G (the most active form of penicillin).To produce penicillin commercially, deep fermentation tanks with the capacity of several thousand gallons are filled with fermentation medium consisting of corn steep liquor, nutrient agar salts, lactose, glucose and phenyl ethanoic acid (phenyl acetic acid).
This medium is inoculated with conidia-suspension of the fungus and is constantly aerated as pellets. The fermentation is completed in 20 hours. When the fermentation is complete, the masses of fungal growth are separated leaving a clear fluid (the broth). The broth is passed over a filter and washed. The filtrate is when mixed with potassium ions, filtered again and dried. The result is a crystalline potassium salt of penicillin G. Penicillin is assayed to determine its potency before being bottled and sold. G in the name ‘Penicillin-G’ refers to ‘Gold Standard’.
(2) Cephalosporin’s:
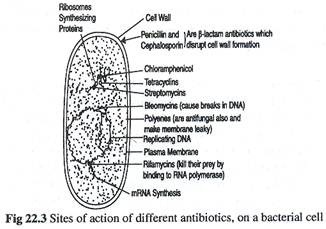
These antibiotics are produced from Cephalosporium acremonium, a marine fungus. They are effective against Gram-negative bacteria. Cephalosporidine, cephaloglycin and cephalexin are some derivative compounds prepared from cephalosporin’s. These antibiotics, like penicillin, block the cell-wall synthesis (Fig. 22.3).
(3) Streptomycin:
This antibiotic is obtained from Streptomyces griseus. Its antibiotic activity was first reported by Waksman in 1944. Streptomycin is a “broad spectrum” antibiotic; inhibits many Gram-negative bacteria, several species of Mycobacterium including M. tuberculosis. It also inactivates bacteriophages.
Streptomycin in commercially produced by the strains of the bacterium in a fermentation medium consisting of soybean meal, glucose and mineral salts. The pH of the medium is maintained at 7.5. The fermentation takes place under submerged conditions at 25 to 30°C for 5-7 days. When the fermentation is complete, the masses of bacterium are separated and the antibiotic is obtained from the fermentation broth using organic solvents.