In this article we will discuss about the role of antibodies and antigens in humoral immunity.
Role of Antibodies:
Humoral immunity is antibody-mediated. It protects body from extracellular pathogenic agents by combining with them to form antigen-antibody complex, leading eventually to their elimination. The antibodies play at least in three different ways in this process of elimination of an antigenic agent.
Firstly, the antibody can bind to the surface epitopes of the antigen making it more susceptible to phagocytosis. This is known as opsonization.
Secondly, the antibody molecule can bind to the antigen forming an antigen-antibody complex which then combines with the complement in a step-wise manner to initiate and facilitate phagocytosis of the antigen.
Thirdly, the antibody can bind to toxin molecules elaborated by microbes making them non-toxic. In a similar manner, antibodies can inactivate free virus particles by combining with the epitopes on viral particles to make them incapable of attachment to host cell membranes.
In opsonization, the Fc-domain of the antibody molecule binds to the receptors on phagocytes and the antigen-binding sites to the epitopes of antigen. Thereby the antigen such as a microbial cell is brought close enough to the phagocytic cell, so that it can be ingested and destroyed by the contents of the phagolysosomes.
Opsonization by antibodies is more effective than by complement (C3b) in case of encapsulated bacterial cells. The capsular material, mostly polysaccharides, prevents interaction with the complement C3b. In contrast, these polysaccharides provoke immune response to produce antibodies that can bind specifically to the capsule, so that the bacterial cells can be effectively opsonized and phagocytosed. Opsonization by antibodies is schematically represented in Fig. 10.25A.
There is another mode of destroying antigens by antibodies which is known as antibody dependent cell-mediated cytotoxicity (ADCC) (Fig. 10.25B). By this method, virus-infected body cells and large parasites which cannot be ingested by phagocytes are eliminated.
The antibodies bind with their antigen-binding sites to the virus infected cells or large parasites by recognizing viral epitopes expressed on the body cells, or the natural epitopes of large parasites, like a helminth. Then the Fc-domains of the antibodies bind to the receptors on phagocytic cells, like neutrophils. Release of toxic chemical mediators from lysosomes of the phagocytes kills the infected body cell or the parasite.
Antibodies can neutralize the toxins liberated by bacteria, like Clostridium tetani, Corynebacterium diphtheriae, Vibrio cholerae etc. by combining with them, so that the toxins are no longer able to bind to their target cells. The antibodies produced in response to toxins are called antitoxins. Exotoxins are generally proteins and endotoxins mostly lipolysaccharides, both of which are strongly antigenic (Fig. 10.25C).
Another major role of antibodies of the IgG and IgM classes is activation of complement by the classical pathway. The role of the secretory form of IgA antibodies in the mucous membranes is to trap any microbial or viral antigen that come in contact with mucin.
The IgA antibodies are anchored in mucin with their Fc domains while their antigen-binding sites remain free to trap any incoming microbe or viral entity, thereby preventing its entry into the deeper layers of the membrane (Fig. 10.25D).
An important feature of all classes of immunoglobulin’s is that any one antibody molecule, whether it is monomeric, dimeric or pentameric, can recognize a single antigenic determinant. It follows, therefore, that for each of the thousands of such determinants which can possibly exist in thousands and thousands of antigens, there is a cognate antibody in the human body.
Also, such an antibody or the antibody producing cell must be present before the body encounters the antigen. In other words, the human body is endowed with the potentiality to produce thousands of antibodies, each having specificity for a different antigenic determinant, to meet the challenge of any antigen that may come across during the lifetime.
As antibodies are proteins, the sequences of their amino acids are determined by DNA. The basis of the great diversity of antibodies is genetical.
While discussing the origin of blood cells, it has been seen that majority of B-lymphocytes produced from stem cells in bone marrow which possess receptors capable of interacting with self- antigens are eliminated by apoptosis and the surviving B-cells which have receptors that do not bind to self-antigens migrate to the secondary lymphoid organs. It is in these organs that the B-cells come to meet the non-self or foreign antigens for the first time.
The question that confronts immunologists at this point is: How — from a large and diverse population of B-lymphocytes each carrying a specific receptor — only those are selected by the antigen which carry specific receptors appropriate to their antigenic determinants?
The outline of the underlying principle of this process was first proposed by Burnet and Medawar in the 1950s in their clonal selection theory (Burnet and Medawar were awarded Nobel Prize in 1960). According to this theory, an immunologically responsive cell can respond to only one kind of antigen (precisely one antigenic determinant or epitope) and this property is acquired before the particular cell encounters the antigen.
Clonal Selection Theory:
It has been estimated that the human body can develop immune response against as many as 100 million or more different antigenic determinants which means that the body can produce as many different clones of B-lymphocytes each carrying a specific receptor. The receptors of B-cells are antibodies which bind to the antigenic determinants.
The clonal selection theory explains how from the multitude of different B-cells, the antigenic determinants select only those which carry appropriate receptors. The basis of this theory is diagrammatically explained in Fig. 10.26.
The diagrammatic representation of clonal selection in Fig. 10.26 is over-simplified. A more precise and modern version of clonal selection is discussed below. In the figure (Fig. 10.26), after capturing an antigenic determinant, the appropriate (cognate) B-cell is activated.
Activation of B-Cells:
For activation of B-cells to proliferate and differentiate into plasma cells, binding with cognate antigenic determinants carried, by antigens is not enough. For majority of antigens, participation of T-cells of the T-helper class (TH-cells) is also essential. Such antigens are, therefore, known as T-dependent. Certain antigens, however, can stimulate B-cells directly without the help of these T-cells and they are known as T-independent antigens.
(a) T-dependent pathway:
The mature B-cells, when they first meet the antigens in the secondary lymphoid organs like lymph nodes and spleen, have receptors in the form of IgM and IgD on their surfaces. The antigen selects the B-cells with cognate receptors.
The selected B-cell then acts like an antigen-presenting cell in that it internalizes the antigen together with the receptor molecules into its cytoplasm and displays the epitopes complexed with MHC class II proteins on its surface. This behaviour of B-cells is unique and is essential for binding to the TH-cells for further activation, because the T-cells are unable to recognize antigens unless they are presented along with MHC proteins.
In the T-dependent B-cell activation, binding of the antigen to the B-cell receptor constitutes the initial step which provides the first signal for activation, but is not adequate. The second signal is provided by its binding to an appropriate TH-cell with its T-cell receptor and the MHC Class II proteins with the epitope embedded in it. The binding between the B-cell and TH-cell is further stabilized by other ligands of both partners.
The bound TH-cell then secretes cytokines, like interleukin-2 which stimulate the B-cell to proliferate and differentiate into antibody-secreting plasma cells (Fig. 10.27). But the picture is not yet complete, because the TH-cell that can bind to the appropriate B-cell needs also to be activated.
The activation of TH-cells is effected by its interaction with an antigen-presenting cell, like a macrophage. Such a macrophage, in the meantime, has engulfed the same antigen which had selected the B-cell and displayed the epitopes complexed with its MHC Class II proteins on its surface. A TH-cell now binds to the macrophage with its T-cell receptor.
This binding is also helped by other proteins ligands, specially the CD4 protein of the TH-cell and the MHC protein of the macrophage. The macrophage secretes cytokines like interleukin-1 which stimulates the TH-cell to become activated and to proliferate producing a clone of activated TH-cells (Fig. 10.28).
One of these activated TH-cells then binds to the activated B-cell and the B-cell is stimulated to become larger in size and to divide producing a clone of antibody-producing plasma cells. A tight binding not only stimulates the B-cell, but also co-stimulates the TH-cell to secrete cytokines, like interleukins 2, 4 and 5 which play vital roles in activation of B-cells.
The plasma cells are short-lived, having a life-span of 3 to 4 days, but they are extremely efficient in antibody synthesis, producing some 2,000 Ig molecules per second. The antibody molecules are secreted into circulatory system. Not all of the activated B-cells are transformed into plasma cells, but a small proportion (about 5%) circulates as memory cells.
An overall picture of T-dependent pathway of B-cell activation leading to antibody production is shown in Fig. 10.29:
(b) T-independent pathway:
There are some antigens which can bind directly to B-cells to induce them to produce antibodies. They do not require participation of TH-cells and, hence, are known as T-independent antigens. These antigens are mostly bacterial surface polysaccharides, like those forming the capsule. The antibodies produced in response to these polysaccharides bind with the capsule to opsonize capsulated bacteria, thereby facilitating ingestion by the phagocytic cells of the body.
T-independent activation of B-cells proceeds via a pathway which is different from that of T-dependent pathway. At high concentration, the polysaccharide antigens can directly interact with the B-cells and activate them to produce antibodies.
The polysaccharide molecules consist of repetitive units. With the help of these units, they can bind to B-cells irrespective of their specific antigenic receptors. The antigen-bound B-cells are induced to proliferate and produce antibody (Fig. 10.30). The T-independent antigens generally induce a weaker response than T-dependent ones. Also no memory cells are the produced in the T-independent pathway.
Interactions Between Antigens and Antibodies:
In humoral immunity, antibodies interact with antigens by their antigen-binding sites to form antigen-antibody complexes. Such complex is formed by actual combination of the two components. An antigen, whether it is a protein or polysaccharide or any other antigenic molecule, or a particulate body, like a microbial cell, always contains a number of antigenic determinants each of which can bind to the antigen-binding site of a cognate antibody.
On the other hand, an antibody molecule has two or more antigen-binding sites. Thus both antigen and antibody are mutually multivalent. When they meet each other — either in vitro or in vivo — each antigen is linked to more than one antibody and, in turn, one antibody is linked to more than one antigen. Through a series of bimolecular interactions, antigens and antibodies produce a lattice or framework with alternating antigens and antibodies leading to formation of an antigen-antibody complex.
The characteristic features of an antigen-antibody complex are discussed below:
(a) Antigen-antibody complex:
The basic principles governing antigen-antibody interaction can be best understood in a simple in vitro system when a soluble antigen is treated with its antiserum (serum containing the specific antibody). The antigen-antibody reaction results in a complex that builds up a lattice which grows in size and is eventually precipitated. When such precipitate is analysed, the proportion of antigen and antibody present in it can be quantitatively estimated.
If, in such an antigen-antibody reaction mixture, the quantity of antigen is gradually increased, keeping the quantity of antibody fixed, and the quantity of precipitate and that of the antibody in the precipitate are determined, it is observed that both the quantities increases gradually until a maximum is reached. With further increase of antigen, the quantity of antibody in the precipitate decreases.
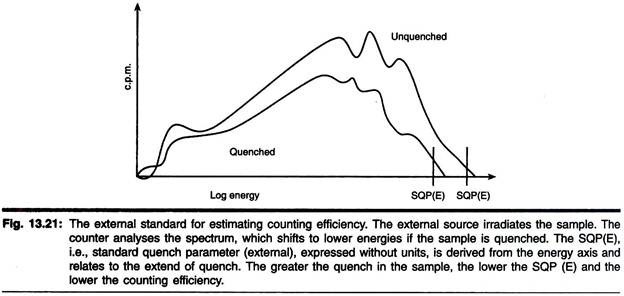
A graphical representation of the antibody present in the precipitate as a function of antigen concentration produces a more or less normal curve as shown in Fig. 10.31:
It is seen from the figure that the precipitate of antigen-antibody complex does not contain a fixed proportion of the two components, as it is expected by the law of fixed proportions applicable to the normal chemical reactions. Rather, the relative proportions of antigen and antibody in the precipitated complex depend on the concentrations of the reactants in the reaction mixture.
Thus, when the antigen concentration in the mixture is low, all the antibody-binding sites of the antigen molecules are engaged, but the antigen-binding sites of all the antibodies are not engaged. This is the antibody excess zone.
As the antigen concentration is gradually increased, more and more of antigen-binding sites of antibodies become engaged. Ultimately, all such sites of the antibody molecules become bound to antigens. This is represented by the equivalence zone.
With further increase of antigen, the binding-sites of all antibodies are engaged but some antigen molecules do not find sites to bind. This is represented by the antigen excess zone of the curve. The supernatant fractions of the reaction mixtures do not contain any free antigen in the first phase (antibody excess zone), neither antigen nor antibody in the second phase (equivalence zone) and no antibody in the third phase (antigen excess zone).
Antigen-antibody complex forming a lattice can be diagrammatically represented as shown in Fig. 10.32:
Antigen-antibody reaction in vivo also results in the formation of complexes, similar to those formed in vitro. At the outset of an infection, only the antigen is present. Antibodies are then produced by plasma cells as a result of immune response. Gradually, antibody concentration increases due to continued production. Interaction of antibody and antigen leads to formation of large complexes as in the equivalence of the in vitro system.
These complexes are generally removed effectively by the phagocytic activity of the polymorphonuclear cells, like neutrophils. Thus, the antigen is destroyed. With the elimination of the antigen, antibody formation slows down due to the absence of antigenic stimulations of the B-cells and finally stops, because the plasma-cells die within 4 to 5 days. Only the memory cells produced in the immune response continue to circulate in the body and can initiate another immune response promptly if the same antigen happens to attack the body.
(b) Antibody-mediated complement activation:
A very important aspect of antigen-antibody interaction is the complement activation by the classical pathway. The complement is a set of constitutive serum proteins which, on activation, performs several important functions including destruction of cellular antigens. Complement activation by the alternative pathway does not involve antibodies, but the classical pathway is dependent on antigen-antibody interaction.
Not all classes of antibodies, but only IgG and IgM can bind complement to their Fc-domain. Such binding can only occur when the antibodies have formed complex with the antigen. Binding of complement to the antigen-antibody complex leads to complement activation by the classical pathway. Such activation eventually leads to lysis of the target cell carrying the antigen. The binding of complement to antigen-antibody complex is known as complement fixation.
In complement activation by the alternative pathway, the components of complement are activated sequentially. This happens also in case of activation by the classical pathway. Complement activation by this pathway begins with binding of an IgM molecule or two adjacent IgG molecules to the antigenic determinants on the surface of the target cell. The target cell is thereby sensitized.
The first complement component, Clq, which is a subcomponent of CI, then binds to the Fc-domain of the heavy chain(s) of the antigen-bound antibody. Clq does not require to be activated, because it has a stable binding site with which it can bind directly to the antibody molecule (Fig. 10.33).
The bound Clq then activates the other subcomponents of CI complex which become catalytically active to cause proteolytic cleavage of the components C2 and C4 to produce C2a and C2b, and C4a and C4b. The fragments C4b and C2a then bind to the target cell forming an enzyme, C3-convertase, which catalytically cleaves C3 component into C3a and C3b.
Next, C3b binds to the target cell surface to form a cell bound complex containing Cl-C4b-C2a-C3b. This complex then activates the binding of the complement components C5, C6 and C7 of which the C5 component is cleaved into C5a and C5b. The fragment C5b is incorporated into the complex which is now Cl-C4b-C2a-C3b-C5b-C6-C7.
Finally, the components C8 and C9 are also added to form the membrane attack complex. This complex is responsible for formation of pores in the membrane of the target cell through which cell contents come out and the cell undergoes lysis. The sequential activation of the complement cascade is shown in Table 10.6 and diagrammatically in Fig. 10.34:
Besides causing cell lysis, the activated complement exert other effects. One important effect is opsonization by the complement fraction C3b which binds both to specific receptors on phagocytic cells and the microbial cell facilitating phagocytosis.
Antibody Diversity:
It has been estimated that human body can produce approximately one billion (109) different antibodies, each having the ability to interact with a specific antigenic determinant. It is also known that antibodies are, proteins of the class immunoglobulin’s and that like other proteins they are synthesized from m-RNA coded by DNA.
The variable domains of H and L polypeptide chains of Ig molecules possess amino acid sequences which are different in each antibody and determine its antigen-binding specificity. The problem that baffled immunologists for a long time is how the human organism having some 100,000 (105) genes manages to produce 109 different proteins.
Dreyer and Bennett (1965) suggested for the first time that the genes encoding the variable and constant domains of Ig molecules are separate in DNA. This meant that the two parts (V arid C) of the same polypeptide molecule are coded by DNA segments which were not continuous. This was not in conformity with the accepted postulate.
The mystery of antibody diversity was solved by Tonegawa and Hozumi when they worked out the mechanism of somatic recombination in 1976 (Tonegawa was awarded the Nobel Prize in 1987). It was shown that the DNA’ segments of H and L chains of Ig molecules were located in different chromosomes and that for each H and L chains were are a number of genes encoding the different domains.
These genes are shuffled to produce a unique set of genes for different H and L chains. The H and L chains are synthesized separately and joined later to produce a monomeric Ig molecule consisting of two identical H chains and two identical L-chains.
The process by which different DNA segments are joined to produce a gene encoding an H or L chain is somatic recombination. This occurs in the embryonic cells when B-cells are differentiated from stem cells. The salient features of antibody-diversity according to the currently accepted views are briefly discussed below.
The genes encoding immunoglobulin’s are distributed in three human chromosomes, viz. genes for H-chains are located in human chromosome 14, those for k-chain (L-chain) in chromosome 2 and those of λ-chain (L-chain) in chromosome 22.
In the DNA of embryonic cells (germ-line DNA) there are many copies of genes encoding the V-domains of H and L chains. The coding segments of these genes are not continuous, but interrupted by non-coding segments (introns).
Besides the genes controlling V and C domains of Ig molecules, other genes code for the joining segments (J) and diversity segments (D).
Thus, an H-chain and an L-chain consist of die following segments:
H-chain: V segment – D segment – J segment – C segment
L-chain: V segment – J segment – C segment.
In the embryonic cells from which B-cells arise, the germ-line DNA contains multiple copies of the genes controlling the V, J, D and C segments. From these genes, one from each segment is selected at random and joined to each other by somatic recombination to yield the DNA of a B-cell. This is known as gene rearrangement or gene translocation. Gene rearrangement of the H-chain is accomplished first and then that of the L-chain is undertaken.
Again, of the two classes of L-chains, rearrangement of the k-chain is taken up first. In case rearrangement of the k-chain DNA fails, then only that of λ-chain is rearranged. As the genes of k-and λ-chains are located in different chromosomes, successful recombination of one chromosome prevents rearrangement of the other chromosome. Thus, it is seen that gene rearrangement in the differentiating B-cells proceeds in a specific order.
In the germ-line DNA, there are some 200 (or more) genes controlling the V segment of the H-chain of Ig molecule, located in chromosome 14. There are also 5 genes for D segment, 9 genes for J-segment and 9 genes for C segment, all located in chromosome 14. Similarly, for the kappa L-chain, there are 80 V genes, 5 J genes and one C gene, located in chromosome 2. The lambda L-chain is also controlled by multiple copies of V genes, J genes and one C gene.
These are shown in Fig. 10.35:
Random selection from some 300 immunoglobulin genes can produce an immensely large number of different antibodies. Thus, the main source of antibody diversity is somatic recombination, though two other factors contribute to it.
A simplified diagrammatic representation of somatic recombination of randomly selected gene segments is shown in Fig. 10.36:
(a) Somatic gene recombination:
In case of L-chains e.g. a kappa chain, recombination starts with joining of one of the VK genes with one of the JK genes, by a process called V-J joining. There are 80 VK genes and 5 JK genes for K-chain. Any one VK gene can be moved to any JK gene. This is controlled by highly conserved nucleotide sequences flanking the genes.
These sequences serve as recombinational signal. These sequences have been determined to be a heptamer and a nonamer separated by a 12 base-pair sequence (spacer) in case of the VK segments and a 23 base-pair spacer in case of JK segment. This unit i.e. a heptamer-spacer-nonamer serves as recognition signal and may precede or follow the coding sequences of the VK and JK genes. These recombinational signal sequences pair with each other and are cleaved to join VK and JK segments. Such pairing of the recombinational signal sequences is possible because the heptamer sequences and the nonamer sequences are exact inverted repeats.
This is diagrammatically shown in Fig. 10.37:
The actual joining of a VK and a JK gene is catalysed by the enzyme recombinase which is formed by two proteins, RAG 1 and RAG 2 (recombination activity gene products). As a result of recombinase activity the two genes are recombined and at the same time, the intervening DNA segments are eliminated in the form of a circle by DNA splicing.
The recombinase nicks each DNA strand at its signal sequence. The nicked ends are rejoined to produce a DNA segment containing a V gene adjacent to a J gene. The recognition signals assure that a VK gene is joined always to a JK gene and not to another VK gene.
Though a VK gene is always joined to a JK gene, the joining process may sometimes result in a loss of a small number of bases from the ends of both VK and J K genes during crossing over of the nicked strands. This imperfect crossing over gives rise to variations in the amino acid sequence of the resulting K-chain. This creates what is known as functional diversity which acts as another source of antibody diversity.
The basic mechanism of gene rearrangement in somatic recombination described with the example of kappa light chain is applicable to other Ig chains, like λ-light chain and heavy chains of different classes of Ig molecules. The DNA segments in all cases are characterized by similar recognition signals consisting of heptamer-spacer-nonamer sequences.
In case of H-chains, there is an extra D segment. During rearrangement, first of all a D segment is joined to one of the J segments producing a D-J combination. Then one of the V genes is trans-located to form a V-D-J combination and lastly, one of the nine C segment is added. Of these nine C segments, there is one for IgM (Cμ), one for IgD (Cδ), four for IgG (Cγ), two for IgA (Cα) and one for IgE (Cϵ).
After the genes of H-and L-chains have been successfully rearranged, the DNA segments are transcribed into a primary transcript (hn-RNA). It contains besides the essential coding segments, also extra segments including introns. These are removed by RNA-splicing to produce an m-RNA.
Translation of the m-RNA takes place on ribosomes attached to the endoplasmic reticulum of the B-cells. The resultant polypeptides of H-and L-chains are secreted into the lumen of E.R. where they combine to form a complete Ig molecule. It is then transported to the B-cell membrane where it is expressed as an antigenic receptor.
The process of gene rearrangement in one L-chain (kappa) and one H-chain (of IgM) is described below:
(b) Generation of kappa L-chain and its polypeptide:
The first step in gene rearrangement of the k-chain is the joining one of 80 V genes (say V 50) to one of the 5 J genes (say J4) in a B-cell. Then the V-J genes are joined to the Ck gene.
The process is shown in Fig. 10.38:
(c) Generation of H-chain of IgM:
Heavy chain generation starts with joining of a D-segment with a J-segment.
The process of H-chain formation of IgM is shown in Fig. 10.39:
The main factor which plays the key role in creating antibody diversity is doubtlessly the random combination of V, D, J and C segments, each of which has few too many representatives in the germ-line DNA. Additionally, the imprecise joining of V, D and J segments (junctional diversity) also is responsible for some diversity. Another factor that adds to antibody diversity is the high rate of somatic mutation of the V genes of germ-line DNA.
Affinity Maturation of Antibodies:
Antibodies produced as a result of secondary immune response generally show a higher affinity to antigens than those produced in the primary response. We know that affinity refers to the firmness of binding of an antibody molecule to its cognate antigen and that it is distinct from valence of an antibody which refers to the number of antigen-binding sites possessed by an antibody molecule. Affinity maturation is the increased affinity of the antibodies produced in the secondary response in comparison to that of primary response.
The higher affinity of antibodies for antigens has been thought to be due to the larger number of antibody-producing cells generated in secondary response which competes with each other for binding to the available antigens. As a result, those B-cells which produce antibodies with higher affinity are favoured by natural selection for proliferation and transformation into antibody-producing plasma cells.
The production of higher-affinity antibodies is due to somatic mutation in the V genes of germ-line DNA. Thus, as the immune response progresses, antibodies appear that bind more effectively due to affinity maturation.
Class Switching:
Class switching refers to the ability of a B-cell to switch over production of one class of antibody to another class, both haying the same antigenic specificity. A B-cell initially expresses IgM and IgD on its surface. After being stimulated, the same B-cell expresses IgG or other antibodies. This is known as class switching. It occurs through interaction of the B-cell with a TH-cell.
TH-cells bind to B-cells with specific proteins ligands. Such binding induces the TH-cell to secrete specific cytokines. Class switching is effected through the cytokines as well as binding with specific ligands of both cells (TH and B).
TH-cells are divided into two main types, TH-1 and TH-2, both being CD4+ cells. While the main function of TH-1 cells is to activate macrophages through production of the cytokine — interferon y, they also induce class switching of B-cells to produce IgG instead of IgM.
The major function of Th-2 cells is in humoral immunity in which they participate in T-dependent antibody formation by B-cells. TH-2 cells secrete cytokines including interleukin-4 and interleukin-5. When a Th-2 cell binds to a B-cell, the latter produces IgE or IgA. Here also, the two cells interact by binding to each other with specific ligands. Binding of TH-1 and TH-2 cells with B-cells associated with class-switching is shown in Fig. 10.40.
The cytokines viz. interferon y, interleukins 4 and 5 are believed to induce differential cleavage and splicing of the primary transcript (hn-RN A) during formation of the H-chains of Ig molecules. As a result a V-D-J segment already formed by gene rearrangement is attached to a different C segment.
The C segment is different in the different classes of Ig molecules e.g. Ig M contains Cμ, IgG contains Cy and so on. As the V-D-J segment coding for the variable domain of the Ig molecule does not change during class switching by the cytokines, the antigen-binding specificity of the antibody is not affected. Thus, though an antibody of the class IgM is changed to IgG or IgA or IgE, it still binds to the same antigen.