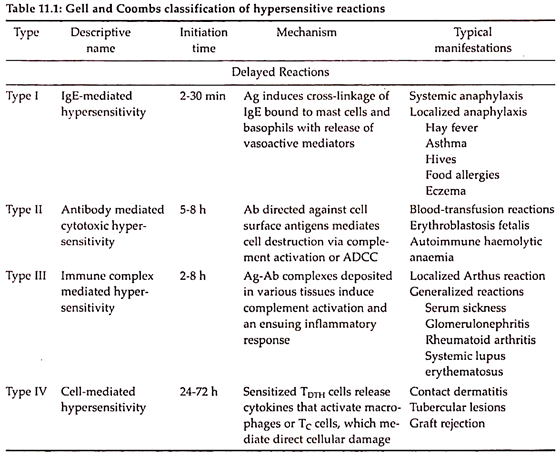
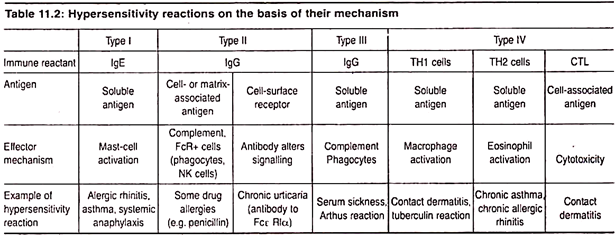
Several types of hypersensitive reactions can be identified, reflecting differences in the effector molecules generated in the course of the reaction. Gell and Coomb described four types of hypersensitivity reactions (Types I, II, III and IV). The first three types are antibody-mediated and the fourth type is mediated mainly by T-cell and macro-phases i.e. cell-mediated (Table 11.1 and 11.2; Fig. 11.2).
1. Type I Hypersensitivity:
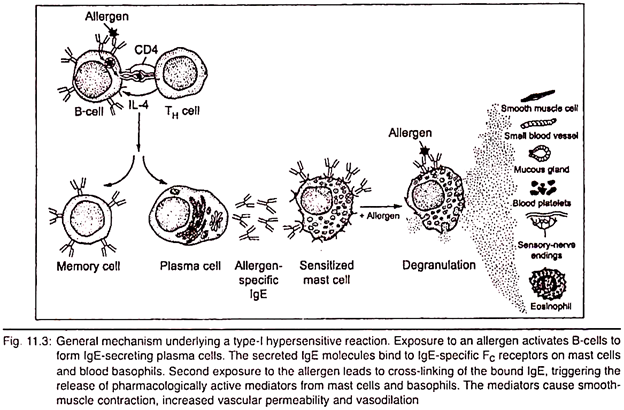
Type I hypersensitive reactions are the commonest type among all types which is mainly induced by certain type of antigens i.e. allergens. Actually anaphylaxis means “opposite of protection” and is mediated by IgE antibodies through interaction with an allergen.
(i) Mode of Action:
During the activity, this class of antibody (IgE) binds with high affinity to FC (Fragment crystalized) receptors on the surface of constant domains of tissue mast cells and blood basophils. Such IgE-coated mast cells and basophils are said to be sensitized. When the individual is exposed to the same allergen again, then it cross-links the membrane bound IgE on sensitized mast cells and basophils and degranulation of those cells result (Fig. 11.3).
(ii) Biological effects:
1. Normally anaphylactic responses are of a mild type producing symptoms— like hay-fever, running nose, skin eruptions called as ‘nives’ or breathing difficulties.
2. The pharmacologically active mediators released from the granules exert biological effects on the surrounding tissues.
3. In some cases, the responses may be severe, develop within a few minutes (2-30 mins) and may even cause death before any medical help is called anaphylactic shock.
4. The principal effects of vasodilation and smooth muscle contraction may be either systematic or localized.
(iii) Components of type-I reactions:
There are different types of components which are required for type-1 reactions:
1. Different allergens
2. Reaginic antibody (IgE)
3. Mast cells and basophils
4. IgE—binding FC receptors.
5. High—affinity and low-affinity receptors.
(iv) Therapy for Type-I hypersensitivity:
1. The first step in controlling type I is to identify the offending allergen and avoid contact if possible.
2. Removal of house pets, dust-control measures.
3. Repeated injections of increasing doses of allergens called hypo sensitization.
4. Enhancement of phagocytosis by IgG antibody which is referred to a blocking antibody because it competes for the allergens, binds and forms a complex that can be removed by phagocytosis.
5. Successful use of anti-histamine drugs result better with respect to type I hypersensitivity.
2. Type II Hypersensitivity:
Type II hypersensitive reactions are those in which tissue or cell damage is the direct result of the actions of antibody and complement.
(i) Mode of action:
This type of reaction is resulted by blood- transfusion reactions in which host antibodies react with foreign antigens present on the incompatible transfused blood cells and mediate destruction of these cells.
Antibody can mediate cell destruction by activating the complement system to create pores in the membrane of the foreign cell by forming membrane attack complex (MAC). This can also be mediated by antibody dependent cell-mediated cytotoxicity (ADCC).
A faulty cross-matching leads to haemolysis of the donor’s erythrocytes in the blood vessels of the recipient due to the alloantigen of the donor’s erythrocytes react with the antibodies in the serum of the recipient and in combination with activated complement, the erythrocytes undergo haemolysis (Fig. 11.4).
(ii) Biological effect:
1. Haemolytic disease of the newborn develops when maternal IgG antibodies specific for foetal blood-group antigens cross the placenta and destroy foetal red blood cells. Severe haemolytic disease of the new born is called erythroblastosis foetalis, when an Rh+ foetus expresses an Rh antigen on its blood cells that the Rh– mother does not express it (Fig. 11.5).
2. Certain antibiotics (e.g. penicillin, cephalosporin and streptomycin) can absorb non- specifically to proteins on RBC membranes, forming a complex similar to a hapten-carrier complex and gradually induces anaemia called drug-induced haemolytic anaemia.
3. Type III Hypersensitivity:
When an antigen enters within the body then the antibody reacts with antigen and generates immune complex. This immune complex gradually facilitates removal of antigen by phagocytic activity of body. Large amount of immune complexes lead to tissue-damaging Type III hypersensitivity. For this reason Type III is called immune complex hypersensitivity.
(i) Mode of action:
1. These reactions develop when immune complexes activate the complement system’s array of immune effector molecules. Complement components (C3a, C4a, C5a) split and produce anaphylatoxins which cause localized mast cell degranulation and increase local vascular permeability.
2. When formed bulky antigen-antibody complexes aggregate and combine with the activated complement, they chemotactically attract the polymorphonuclear leucocytes. These cells release lysosomal enzymes in large quantities to cause tissue damage.
(ii) Biological effect:
1. The recipient of a foreign antiserum develops antibodies, specific for the foreign serum proteins from circulating immune complexes and within days or weeks after exposure to foreign serum antigens, an individual starts to develop serum sickness including fever, weakness, vasculitis (rashes) with edema, erythema, lymphadenopathy, arthritis and glomerulonephritis.
2. Due to deposition of IgG antigen complexes in the blood vessels cause local damage and deposit in blood vessels of kidney glomeruli called Arthus Reaction.
3. Inhalation of bacteria and fungal spores gives rise to a disease called farmer’s lung forming immune complexes in the epithelial layers of the respiratory tract.
4. Another type of hypersensitive reaction is known as lupus i.e. systemic lupus erythematosus. It is produced as a result of interaction of IgG and the nucleoproteins of the disintegrated leucocytes (auto-antigens). Lupus is an autoimmune disease.
4. Type IV Hypersensitivity:
Type IV hypersensitivity is the only type of delayed hypersensitivity. It is mainly controlled by T-cells, macrophages and dendritic cells. It is not the instant response but it is manifested after the second exposure to an allergen. The appearance of allergic symptoms come in delay.
(i) Mode of action:
Delayed hypersensitivity is maintained by T- lymphocytes. T-cells (lymphocytes) have two main types—the CD4+ cells and CD8+ cells. Type IV hypersensitivity requires CD4+ type. The special group of CD4+ cells take part in type IV hypersensitivity and are called T-D cells (delayed). Again T-helper cell (TH cell) includes T-D cells which constitutes the bulk of CD4+ T-cells. TH cells are again distinguished into TH-1 and TH-2 type, of which TH.2 cells are mainly responsible for activation of B-cell to produce immunoglobulins and TH-1 cells are involved in causing the inflammatory responses including delayed hypersensitivity reactions (Fig. 11.6).
(ii) Biological effect:
1. A microbial agent that elicits a delayed hypersensitivity is tuberculin which is a purified protein derivative (PPD) of tubercle bacilli (Mycobacterium tuberculosis). Mycobacterium leprae, the microbial agents also stimulate delayed hypersensitivity.
2. The tuberculin skin test (Mantoux test) is used to determine if a person has T-cell mediated reactivity towards tubercle bacilli (also known as Koch’s bacilli).