The following points highlight the three main types of immunity present in humans. The types are: 1. Innate (Natural or Nonspecific) Immunity 2. Acquired (Specific or Adaptive) Immunity 3. Active and Passive Immunity.
Contents
Type # 1. Innate (Natural or Nonspecific) Immunity:
Innate immunity (also called nonspecific or natural immunity) refers to the inborn-ability of the body to resist, and is genetically transmitted from one generation to the next. This immunity offers resistance to any microorganism or foreign material encountered by the host.
It includes general mechanisms inherited as part of the innate structure and function of each vertebrate, and acts as first line of defence. Innate immunity lacks immunological memory, i.e., it occurs to the same extent each time a microorganism or foreign material is encountered.
Types of Innate Immunity:
Innate immunity can be divided into species, racial, and individual immunity.
(i) Species Immunity:
Species immunity (species resistance) is that in which a disease affecting one species does not affect the other species. For convenience, humans do not contract cattle plague, chicken cholera, hog cholera, infectious horse anaemia, etc., while animals are not affected by many human diseases such as enteric fever, scarlet fever, syphilis, gonorrhoea, measles, etc.
Diseases of skin, to which humans are quite susceptible, are often resisted by animals because they have more hair and thicker hides. Species resistance is considered to be the result of a long evolution of interactions between the highly evolved “macro” organisms and the pathogenic microorganisms.
(ii) Racial Immunity:
Racial immunity (racial resistance) is that in which various races (breeds) show marked differences in their resistance to certain infectious diseases. A well known example is that Brahman cattle are resistant to the protozoan parasite responsible for tick fever in other breeds of cattle. Similarly, Black Africans affected by sickle cell anaemia, a genetic disease, are resistant to malaria while malaria affects other human races.
(iii) Individual Immunity:
Having the same racial background and opportunity for exposure, some individuals of the race experience fewer or less severe infections than other individuals of the same race. For convenience, children are more susceptible to diseases such as measles and chicken pox, while aged individuals are susceptible to other diseases like pneumonia.
Type # 2. Acquired (Specific or Adaptive) Immunity:
Acquired immunity (also called specific or adaptive immunity) refers to an immunity that is developed by the host in its body after exposure to a suitable antigen or after transfer of antibodies or lymphocytes from an immune donor.
Characteristics of Acquired Immunity:
Acquired immunity is highly adaptive and is capable of specifically recognizing and selectively eliminating foreign microorganisms and macromolecules, i.e., antigens.
It exhibits the following four characteristic features that distinguish it from nonspecific (innate) immunity:
(i) Specificity:
Acquired immunity is extremely antigenic specific as it acts against a particular microbial pathogen or foreign macromolecule and immunity to this antigen usually does not confer resistance to others. For convenience, the ability of the antibodies to differentiate between antigen molecules differs even by a single amino acid.
(ii) Diversity:
The acquired immune system generates tremendous diversity in its recognition molecules. As a result, it is able to specifically recognise billions of different structures on foreign antigens.
(iii) Memory:
Once the acquired immune system has recognised and responded to an antigen, it is able to respond this antigen more quickly and strongly following a subsequent exposure. This is due to the constitution of immunologic memory that makes the basis for long-term immunity in the body of the host.
(iv) Discrimination between “Self’ and “Nonself”:
The immune system almost always recognizes self and nonself antigens and responds only to nonself antigens. This ability to recognize self antigens from nonself ones is critical for normal functioning of the immune system. Sometimes this feature fails and, as a result, there develops autoimmune disease in the host.
Major Functions of Acquired immunity:
The acquired (specific or adaptive) immune system of the body is required to perform the following three major functions:
(i) It has to recognize any thing that is foreign to the body. The foreign material is called “nonself”. The recognition system of acquired immunity is so highly specific that it is able to differentiate one pathogen from another, cancer cells, and even body’s own “self” proteins from foreign “nonself” proteins.
(ii) After recognizing the foreign invader, the acquired immune system responds to this invader by recruiting its defensive molecules and cells to attack the invader. This response, called effector response, either eliminates the invader or makes it harmless to the host and thus protects the body from disease.
(iii) The acquired immune system remembers the foreign invader even after its first encounter. If the same invader attacks the previously attacked body at a later time, the system remembers the invader and mounts a more intense and rapid memory or anamnestic response, which ones again eliminates the invader and protects the host from disease.
Components of Acquired Immunity:
Acquired immunity involves the following two major groups of cells:
(1) lymphocytes and
(2) antigen-presenting cells (APCs).
Lymphocytes are one of the many types of white blood cells (leucocytes) generated in bone marrow by the process of hematopoiesis. They migrate from bone marrow, circulate in the blood and lymphatic system, and reside in various lymphoid organs.
Lymphocytes possess antigen-binding cell-surface receptors and are responsible for the specificity, diversity, memory, and self/nonself recognition by the immune system.
In contrast, antigen-presenting cells (APCs) have class II MHC (major histocompatibility complex) molecules on their plasma membrane. These MHC molecules bind to antigen-derived peptides and present them to a group of lymphocytes, which are then activated to mount the immune response.
Collaboration between Innate and Acquired Immunities:
Although the acquired immunity develops after exposure to a suitable antigen or after transfer of antibodies or lymphocytes from an immune donor, it is not independent of innate immunity which is an inborn ability in the body.
Both the immunities function as a highly interactive and cooperative system rendering a combined response more effective than either immunity could produce by itself. It so happens because certain immune components play significant role in both types of immunities.
Following are the examples that show the interactive and cooperative roles of the two immunities:
(i) Phagocytic cells crucial to innate immunity are intimately involved in activating acquired immunity. Interactions between receptors on phagocytic cells and microbial components generate soluble factors that stimulate and direct acquired immunity facilitating the participation of the system in the elimination of the foreign invader. Acquired immune system, in turn, produces signals and components that stimulate and inhance the effectiveness of innate immunity.
(ii) Stimulated phagocytic cells involved in innate immunity also secrete cytokines that direct acquired immunity against particular intracellular microbial pathogens. In turn, some T lymphocytes of acquired immunity synthesize and secrete cytokines that increase the ability of phagocytic cells to destroy the microbial pathogens they have phagocytized during innate immune responses.
Differences between Innate and Acquired Immunities:
In contrast to their interactive and cooperative nature, the innate and acquired immunities show certain fundamental differences, which are the following:
(i) Innate immunity shows rapid response in comparison to acquired immunity the response of which is slower.
(ii) Innate immunity utilizes a pre-existing but limited repertoire of responding components, whereas the acquired immunity possesses ability to recognize a much wider repertoire of foreign substances.
(iii) Innate immunity remains constant during a response, whereas the acquired immunity possesses ability to improve during the response. It may be emphasized that due to its immunological memory, the acquired immunity operates much faster to the same pathogen during secondary exposure than the primary exposure.
These fundamental differences between innate and acquired immunity can be consolidated in the form of Table 41.2.
Types of Acquired Immunity:
Acquired immunity can be obtained by the host actively or passively and, on this basis, can be categorized as of two types:
(i) Active immunity and
(ii) Passive immunity.
In active immunity, there is active involvement of host’s own immune system leading to the synthesis of antibodies and/or the production of immuno-competent cells (ICCs).
In passive immunity, on the contrary, the antibodies and /or the immuno-competent cells (ICCs) are transferred from one host to another. Active and passive immunities can be obtained naturally or artificially (Fig. 41.1).
Branches or Arms of Acquired Immunity:
Acquired immunity consists of two branches or arms recognized as:
(i) Humoral and
(ii) Cellular immunity.
Humoral immunity is based on the action of soluble proteins called ‘antibodies’ whereas cellular immunity is based on the action of specific kinds of ‘T lymphocytes’.
Type # 3. Active and Passive Immunity:
1. Active Immunity:
Active immunity, as stated earlier, refers to an immunity in which there is active involvement of host’s own immune system leading to the synthesis of antibodies and/or the production of immunocompetent cells (ICCs).
There are two types of active immunity:
(i) Naturally acquired active immunity and
(ii) Artificially acquired passive immunity.
(i) Naturally Acquired Active Immunity:
This immunity develops after antigens (e.g., microbial pathogens) enter the body by natural processes such as infection and, in response, the body’s immune system forms antibodies.
In some cases, the immunity may be life-long as with smallpox, measles, chickenpox, yellow fever etc. In other cases, however, the immunity may be lost after only a few years (e.g., diphtheria, tetanus) or even for lesser period (e.g., influenza, pneumonia).
(ii) Artificially Acquired Active Immunity:
When a carefully chosen antigen (e.g., vaccine, chemically altered toxins called toxoids) is intentionally introduced into a body to be immunized, the latter develops immunity that is called artificially acquired active immunity. This immunity is artificial because the antigens are intentionally or purposely introduced, and it is active because the recipient’s immune system synthesizes antibodies in response.
Vaccines provide usually long-term immunity. Vaccines are now available against many infectious diseases such as cholera, tuberculosis, plague, pneumonia, rocky mountain spotted fever, smallpox, polio, tetanus, influenza, measles, rabies, yellow fever etc. Toxoids are currently available for protection against diphtheria and tetanus, the two diseases whose major effects are due to toxins.
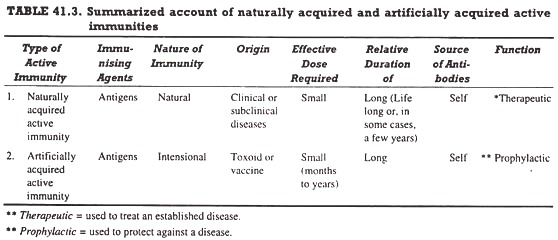
The characteristics of naturally acquired and artificially acquired active immunities are summarized in Table 41.3.
2. Passive Immunity:
Passive immunity, as stated earlier, refers to an immunity in which the antibodies and/or immuno-competent cells (ICCs) are transferred from one host to another.
There are two types of passive immunity:
(i) Naturally acquired passive immunity and
(ii) Artificially acquired passive immunity.
(i) Naturally Acquired Passive Immunity:
When antibodies produced in the body of an individual (called “donor”) are naturally transferred into the body of other individual (called “recipient”), the latter develops immunity, called naturally acquired passive immunity, in its immune system.
This immunity is natural because the transfer of antibodies from donor to recipient occurs under natural conditions, and it is passive because the recipient does not synthesize antibodies but picks them up from the donor.
The best example of this type of immunity is the natural transfer of antibodies from the mother to the foetus across- the placenta. Certain antibodies are also transferred from mother to infant through colostrum and milk during nursing.
These antibodies, called maternal antibodies, remain with the child for about three to six months or, sometimes, twelve to fifteen months, and after the specified time the immune state disappears. The maternal antibodies generally provide resistance against whooping cough, diphtheria, german measles, diseases of respiratory and gastrointestinal tract, etc.
(ii) Artificially Acquired Passive Immunity:
Artificially acquired passive immunity is that which develops as a result of the intentional introduction of antibody-rich serum (blood plasma devoid of clotting factors) taken from diseased individual to another susceptible individual.
It was an important therapeutic device for disease treatment before the vaccines were developed and is still used for viral diseases such as hepatitis B, chicken pox, arthropod-borne encephalitis, and for bacterial diseases such as botulism, diphtheria, tetanus, staphylococcal-poisoning where toxins are involved in disease causation.
Since these diseases are very dangerous and fatal, already-made antibodies present in serum are introduced into the blood of the susceptible individual for quick response and no risk is taken for introduction of antigens. Artificially acquired passive immunity is immediate but short-lived (only for two to three weeks).
The characteristics of naturally acquired and artificially acquired passive immunities are summarized in Table 41.4.