In this article we will discuss about:- 1. Occurrence of Lung Fluke 2. Geographical Distribution and Habitat of Lung Fluke 3. Development Phases.
Occurrence of Lung Fluke:
P. westermani, the ‘lung fluke’, occurs in the lungs of various mammals including man and more rarely in the brain, spinal cord and other organs of the pig, dog, cat, goat, cattle, fox, rat, etc. They are commonly called “lung flukes”.
First species to be described was P. westermani from Royal Bengal Tigers and first human species obtained was named P. ringeri. It is still uncertain whether the two species named above are distinct or are the same species.
Westerman (1877) got 2 worms from the lungs of Royal Bengal Tiger and Ringer (1879) recovered similar worms from the first human specimen of Formosa. Cobbold (1880) identified these worms and termed as Distoma ringeri. Manson and Baelz (1880) also observed same type of worms.
Later on Nakgawa (1915-19), Yokogawa, Koboyashi (1918-21) worked out the life cycle of these species. Ameel (1936) worked out the developmental pattern of these worms. Useful reviews of P. westermani and of paragonimiasis are those of Yokogawa (1965, 69) and Bunnag and Harinasuta (1984).
Geographical Distribution and Habitat (Site of Infection) of Lung Fluke:
Geographical distribution:
They have been reported from Far East, Japan, China, Philippines, New Guinea, and Africa etc. In India it is reported from Bengal, Assam and Madras. P. westermani was originally found in the tiger, P. ringeri in man from China and Japan, and P. kellicotti was found in the cat, pig and dog in U.S. and in the cat in South Africa. In U.S.A. it is probable that the mink is the natural host. A survey by Gesinki (1964) showed 35.48% of these animals to have been infected in Ohio.
Habit and Habitat:
i. Adult worms reside in the respiratory tract (lung) of man.
ii. Miracidium and Cercarial stages are present in soft tissues of first intermediate host (snails).
Metacercaria is found in gills, legs or appendages, pericardium, muscle of second intermediate host (crustacea specially crab and crayfish). Yagore et al (1958) observed Metacercaria in the heart or gills of the crab.
The adult Lung flukes live normally in the lungs of definitive hosts, where shortly after they have arrived, the host forms cyst-like pockets around them. Practically the fertilization occurs within the host body. The eggs are laid in the cysts, in which the worms live and escape through connecting channels into the bronchi, or else when the cysts rupture.
The lung cysts in which the worms most commonly occur usually contain 1-3 flukes. The eggs are freed into the bronchial tubes and pass out with sputum, which has a characteristic rusty colour. Animals usually swallow the mucus, and hence the eggs are found in the faeces.
Development Phases of Lung Fluke:
Structure of the Fertilized Eggs:
The fertilized eggs are golden brown in colour, oval in shape and are provided with opercula. They measure 80-118 μm in length by 48-60 μm in diameter and each egg contains an un-segmented ovum surrounded by yolk cells.
Development of Miracidium:
In water, a ciliated embryo develops inside the egg in 2 to 7 week’s-time. A change in temperature and light generally induces hatching but the process does not appear to take place easily. Under suitable conditions eggs hatch into Miracidia into surrounding water. Miracidia develop in the eggs slowly after they leave the body, requiring at least 3 weeks, during which time the eggs must be kept moist (Fig. 9.4).
Infection of the Intermediate Host and Formation of Sporocyst, Redia and Cercaria:
On attaining maturity, the Miracidium escapes into water and swims about in search of an intermediate host (snail host), a species of the genus Melania. The molluscan hosts vary with locality. The most important host is probably Semisulcospira libertina (S. bensoni); others implicated are Melania amurensis, M. obliquegranosa and Brotia asperata.
It is known that life cycle involves two intermediate hosts. First intermediate host is a suitable amphibious snail into which Miracidia enter. Earlier larval stages are passed in it. Inside the soft tissue of the snail the Miracidium casts off its tail and changes into sac like Sporocyst which produces about 12 first generation redial larvae; they in turn produce a similar number of second- generation Redia larvae, being transformed into Cercariae.
Each Redia larva produces 20 or 30 fully developed creeping Microcercous Cercariae. These are 175 to 240 μm long, having a small knob-like tail, spiny cuticle, a stylet and 14 penetration glands. These Cercariae appear within 78 days or more after infection of the snail. They do not swim, but creep in a leech like manner or float with the current.
These Cercariae escape from the snail into water and enter into second intermediate host, a fresh water crab or crayfish. Inside the crustacean host they become encysted in the viscera muscles and gills because they penetrated the body at various vulnerable sites.
The Meta-cercarial cysts are nearly round and are 0.5 mm or less in diameter. The enclosed spiny Metacercariae lie straight, unlike most encysted forms, and are characterised by the presence of large excretory vesicle filled with retractile granules, with large convoluted intestinal caeca on either side.
Development in Final Host:
The Metacercariae escape from the crustacea when these are injured and may live in water for 3 weeks. Man (primary host) and other susceptible hosts get infection by consuming the raw flesh of an infected crab or Cray-fish.
The cyst wall is dissolved by the gastric juice and the Adolescaria is released into the duodenum. After being liberated in the intestine the young fluke penetrates through the wall and wanders through the peritoneal cavity and diaphragm in about four days, entering the lungs from pleural cavity in about 14-20 days.
They may also enter into other organs, such as the brain, from this location. It arrives in the bronchioles, when the host forms a cyst wall around it and grows into adult. Practically in the lungs, a fibrous capsule is formed by the host; after about 6 weeks the worms mature and produce eggs.
Eggs are discharged into a bronchiole and are coughed out with the sputum. The cycle is thus repeated. The pathology of Paragoniamiasis has been reviewed by Bunnag and Harinasuta (1984).
Synapsis of Life Cycle:
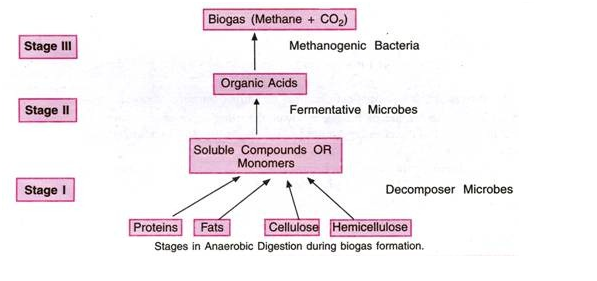
Eggs ––> 2-7 weeks ––> Miracidium larva (in first intermediate host) ––> Sporocyst larva (in first intermediate host) ––> Redia larva (in first intermediate host) ––> Cercaria larva (in second intermediate host) –––> 6 weeks or more ––> Metacercaria (infective stage in definitive host i.e., man etc.).
Causes of Excystment:
The Metacercaria is covered by a cyst-wall of about .01 – .02 mm in thickness. The experiments of Yokogawa (1965) proved the Metacercaria inside the cyst becomes active in gastric juice and after 3-4 hours they die. When put in hot water some of the worms come out of the cyst. Temperature may be the cause for the breaking of the cyst. Oshima (1956-58) found that temperature, pH and osmotic pressure are responsible for the release of the parasites from the cyst.
Speciation of Paragonimus:
Although Paragonimus westermani is regarded as the specific name for this worm in the medical bulletin, but there is evidence that P. westermani occurs in two forms, one of which is diploid (2n = 22) and can be recognised as the true P. westermani and the other which is triploid (3n = 33).
The triploid form, which was collected from Korea, should be recognised as an independent species, P. pulmonalis. The presence of triploid form was observed by Sakaguchi (1975), Tada (1976) and Terasaki (1977). It was found that the karyotype of P. westermani, collected from the Akita Prefecture in Japan, was diploid (2n = 22).
Cytological studies of gametogenesis and embryonic development were carried out on the species P. iloktsuenensis (from rats) and P. sadoensis (from dogs and rats) and it was revealed that both the species were shown to have normal diploid karyotype.
By starch-gel electrophoresis experiment it is revealed that there is a marked difference in the isoenzyme patterns of five enzymes between the diploid and triploid forms. Ultra-structural differences in Metacercarial cyst wall have also been noticed by Higo and Ishii (1987). These differences seem sufficient to conclude that two distinct species, P. westermani and P. pulmonalis, should now be recognised.
Symptoms and Pathogenicity of Paragonimiasis:
Infection with P. westermani is known as Paragonimiasis. It may be divided into two groups— Pulmonary and Extra-pulmonary Paragonimiasis.
The symptoms of Pulmonary paragonimiasis are bronchitis with morning cough, sputum with blood, slight temperature and fatigue.
Pulmonary symptoms are chronic cough, which becomes worse in the morning with rusty or purulent sputum and haemoptysis which is slight but may be severe. Signs of pneumonia or tuberculosis is noticed.
Symptoms of Extra-pulmonary paragonimiasis:
In case of abdominal organs the symptoms include pain in the abdomen, diarrhoea and enlargement of the liver. In cerebral infection, Jackonian type of epilepsy and characteristic brain tumour develop.
The other symptoms are slight temperature, fever, anaemia, generalized lymphadenitis, and cutaneous ulceration.
Pathogenicity:
The parasites in the lungs are not usually of great importance, but those lodged in the brain and other organs may cause trouble.
Mode of infection:
Infection is effected by ingestion of raw or improperly cooked flesh of an infected crab or Cray-fish.
Infecting agent:
Metacercaria or adolescaria inside a cyst.
Portal of entry:
Alimentary canal.
Prophylaxis and Treatment of Paragonimiasis:
Prophylaxis:
1. Prevention of infection consists either in the destruction of the snails that serve as intermediate hosts; abstaining from the use of raw crabs or crayfish for food or of their juices as home remedies.
2. Disinfection of the sputum and faeces.
Treatment:
1. Emetine hydrochloride together with sulfonamides is sometimes effective in treatment.
2. Chloroquine is effective if given relatively early, but after the formation of heavy cysts the drug fails to reach the flukes.
3. Bithionol and Niclofolen have been found to give encouraging results.
4. Removal of patients from endemic areas is suggested.