Here is a list of seven major protozoan diseases: 1. Toxoplasma Gondii 2. Plasmodium 3. Balantidium Coli 4. Trichomonas Vaginalis 5. Giardia Lamblia 6. Trypanosoma 7. Entamoeba Histolytica.
Protozoan Disease # 1. Toxoplasma Gondii:
Toxoplasma gondii is an intracellular parasitic sporozoan (Fig. 24.1). It causes a disease known as toxoplasmosis when transmitted either from soil or other animals (e.g. domestic cats). The exact nature and life cycle of T. gondii are not known (Fig. 24.2).
The oocytes of the parasite released from faeces (of infected cats, horses, sheep, goats, swine) are inhaled or engulfed by human or other animals. The sporozoites emerge as trophozoites which can reproduce in tissues of a new host.
After infection in adults symptoms may or may not develop. However, the minor symptoms resemble with that of viral influenza or mononucleosis. The most remarkable symptom develops in pregnant women where the parasite crosses the placenta within three months of pregnancy, and established inside the foetus resulting in infection of uterus.
Finally, it results in congenital abnormality or stillbirth of a child. However, if the women are infected at later stages of pregnancy, symptoms occur. During pregnancy about 1% women get infected and about 25% infants after birth show symptoms. Therefore, at this stage the pregnant women should be careful about the cats. Oocytes in their faecal material must be checked.
In addition, when the pathogen is outside the foetus, it migrates to intracellular macrophages, gets established as intracellular parasite, becomes centered in the central nervous system and causes encephalitis.
Examination of tissues and T. gondii is useful for diagnosis of toxoplasmosis. Antibodies may be detected by ELISA and direct fluorescence tests. To control the infection anti-protozoan drugs e.g. pyrimethamine should be given in combination with sulfonamides.
Protozoan Disease # 2. Plasmodium:
Plasmodium is a common spore-forming sporozoan parasite on human which causes malaria. Until 1935, malaria was a common disease in humans creating a serious problem and causing death en masse. But with the development of awareness and research programmes, antimalarial drugs were formulated.
Still in African and Asian countries including India, malaria has not been fully eradicated despite of efforts from Government organizations. As per recent estimates about 300 million people suffer from malaria and about 2-4 million die each year. Four pathogenic species of Plasmodium viz., P. vivax, P. falciparum, P. malariae and P. ovale have been recognised. P. falciparum is the most dangerous species followed by P. vivax.
Protozoan Disease # 3. Balantidium Coli:
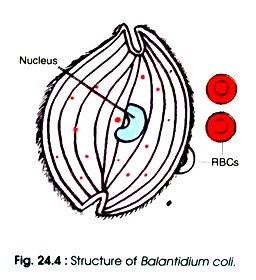
Balantidium coli causes balantidiasis or balantidial dysentery. It is the only largest and ciliated pathogenic protozoan of human intestine (Fig. 24.4). B. coli enters in the intestine when its cysts present in contaminated food or water are ingested by humans. After ingestion the parasite reaches to the colon, wall of cysts dissolved and trophozoites are released.
The trophozoites feed upon bacteria, faecal debris and tissue of colon. When the faeces get dehydrated and pass through colon, the parasite becomes encysted, discharged through faeces and contaminate the water and food. In colon, the parasite remains in two forms i.e. vegetative form (trophozoite) and cyst form.
It lives in large intestine and rarely invades the epithelial lining and cause abdominal cramping, vomiting, weight loss. Due to invasion of epithelium, there develops ulcer in large and small intestines with total dysentery. The cysts can be observed upon microscopic observation of faeces. Life cycle of B. coli is shown in Fig. 24.5.
Protozoan Disease # 4. Trichomonas Vaginalis:
Trichomonas vaginalis is an inhabitant of vagina and urethra (Fig.24.6). It grows and increases its number over the normal microbial community, when acidity of vagina is disturbed from normal pH (3 8-4 4). The change in pH of vaginal fluid may be due to a loss of normal acid-producing bacterial flora or use of oral contraceptives.
In such situation, it causes trichomoniasis or ‘trich’ in female and rarely in males. T. vaginalis is also transmitted by sexual intercourse or contaminated examination tools, towels, catheters, etc. After infection, it causes a mild inflammation of vagina, cervix and volva. It renders the dissolution of infected surface tissues. Consequently, a yellow or cream-white ooze of foul odour comes out.
This type of disease is also caused by Candida albicans and Gardnerella vaginalis. In males, the prostate, seminal vesicle and urethra may be infected and consequently discharge a white liquid. T. vaginalis is observed under the microscope by taking the samples from the discharged fluid.
The parasite is also found in semen or urine in males. Effective treatment is the use of oral metronidazole (flagyl), and the other anti-protozoan drugs.
Protozoan Disease # 5. Giardia Lamblia:
Giardia lamblia is a flagellated (8 flagella) protozoan parasite of human intestine (Fig.24.7) that causes the prolonged diarrhea in humans called giardiasis. It is a water-borne disease occurring throughout the world. The parasite is found in human faeces. The flagella of G. lamblia help to attach firmly at the intestinal wall of human.
It does not infect the intestinal wall but increases its number in the lumen and interferes the food absorption. A large number of cysts are formed which are released with faeces. This disease persists for about a week. It is characterised by malaise, nausea, weakness, weight loss and internal cramps with cronic greasy diarrhoea. The greasy consistency of faeces is the key feature of giardiasis.
About 7% of total population is carriers of this disease. In addition, wild mammals especially beavers also shed the cysts into faeces which in turn contaminate water. The encysted protozoa is resistant to chlorine. Therefore, filtration of water supply becomes very important for elimination of cysts from water. Effective chemotherapeutic agent for giardiasis is the use of metronidazole or quinacrine hydrochloride.
Protozoan Disease # 6. Trypanosoma:
Trypanosoma is known as haemo-flagellate because it infects the blood. Disease caused by the parasite is known as trypanosomiasis or sleeping sickness. T. gambiense and T. rhodosiense cause African sleeping sickness, whereas T. cruzi is responsible for changes disease i.e. American trypanosomiasis. Wild animals such as rodents, opossums and armadillos are the reservoir for T. cruzi.
The arthropod vectors are the kissing bug and the bed bug (Cimex lectularis). T. gambiense and T. rhodosiense are transmitted by Glossina, the tsetse fly. The kissing bug bites the person near the lips. The trypanosomes grow inside the gut of bugs. When the bugs defecate during feeding, the bitten human often rubs the faeces into the wound of the other abrasions of skin or eyes.
The parasite passes through the several stages of life cycle at the site of inoculation. At the inoculation site i.e. commonly near the eyes a swollen lesion develops. The pathogen infects the lymph and is carried by the blood to the other part of body organs such as spleen, liver and heart.
In response to the parasite when inflammation occurs, it damages the macrophages and central nervous system. The loss of tissue progresses that leads to weakness, loss of appetite and apathy. Patients usually fall into coma and finally die. At this stage control of chaga’s disease is very difficult. Laboratory diagnosis can be done by observing the parasite in blood (Fig. 24.8).
Protozoan Disease # 7. Entamoeba Histolytica:
The name of pathogen itself defines the disease (ent=inside, amoeba=varied shape, histo= tissue, lytica- bursting). It causes amoebiatic dysentery i.e. amoebiasis throughout the world. The parasite spreads through the contaminated water or food. The normal level of chlorine does not kill the amoeba.
The cysts are not affected by the acid of stomach i.e. HCl. Only the vegetative cells are destroyed. On the epithelial cell of the wall of large intestine the vegetative cells multiply. This results in severe dysentery where the faeces contain mucus and blood. The life cycle of E. histolytica is given in Fig. 24.9.
The pathogen feeds upon RBCs and damages the tissue of gastrointestinal tract. During severe cases, amoebae may enter the tissues of vital organs and cause abscess in liver, lungs, intestinal wall, etc.
The intestinal wall becomes perforated. If abscess is formed it is treated surgically. The pathogen is identified by observing the amoebae in faeces and RBCs in trophozoites. Effective chemotherapeutic drugs are metronidazole plus iodo-quinol.