In this article we will discuss about the normal microflora of different parts of human body.
Normal Microflora of the Skin:
An average adult human is covered with approximately 2 m2 of skin. It has been estimated that this surface area supports about 1012 bacteria. The skin (Fig. 44.1) surface (epidermis) is not a favourable place for abundant microbial growth, as it is subject to periodic drying.
Most skin microorganisms are associated directly or indirectly with the apocrine glands (sweat glands), which are secretary glands occurring mainly in the underarm and genital regions, the nipples, and the umbilicus. Underarm odour develops as a result of bacterial activity in the apocrine secretions.
Similarly, each hair follicle is associated with a sebaceous gland, which secretes a lubricant fluid. Hair follicles provide an attractive habitat for microorganisms in the area just below the surface of the skin. The secretions of the skin glands are rich in microbial nutrients such as urea, amino acids, salts, lactic acid, and lipids.
The representative genera of microorganisms that inhabit the skin are—Acinetobacter, Enterobacter, Klebsiella, Corynebacterium, Micrococcus, Propionibacterium, Proteus, Pseudomonas, Staphylococcus, Streptococcus, Bacillus, Mycobacterium (occasional), Malassezia, Pityrosporum, and Candida. The last three of the list are micro-fungi.
Although the resident microflora remains somewhat constant, various factors influence its normal composition.
These factors are:
(i) The weather that may cause an increase in skin temperature and moisture, which increases the density of the skin microflora,
(ii) The age of the host that has an effect, and young children have a more varied microflora and carry more potentially pathogenic gram-negative bacteria than adults, and
(iii) Personal hygiene that influences the resident microflora, and unclean individuals usually have higher microbial population densities on their skin. Microorganisms that cannot survive on the skin generally succumb from either the skin’s low moisture content or low pH.
Normal Microflora of the Oral Cavity:
The normal microflora of the oral cavity (mouth) consists of microorganisms that possess ability to resist mechanical removal and firmly adhere to surfaces like gums and teeth.
The normal microbial population able to colonize the mouth finds a very comfortable environment due to the availability of food particles and epithelial debris as nutrients, water, the suitability of pH and temperature, and the presence of many other growth factors.
The oral cavity or mouth is totally free of microorganisms at the time of birth, but it is colonized by microorganisms from the surrounding environment within hours after a human baby is born. In the beginning the microbial flora that establish in the mouth belong to the genera Streptococcus, Neisseria, Actinomyces, Veillonella, Lactobacillus, and some yeasts. These initial microorganisms are aerobes and obligate anaerobes.
When the first teeth erupt, the anaerobic forms (e.g., Porphyromonas, Prevotella, Fusobacterium) dominate as the space between the teeth and gums is anaerobic. Later on, Streptococcus spp. come on to the enamel surfaces of teeth, and also attach to the epithelial surfaces and colonize saliva.
The presence of these bacteria contributes to the eventual formation of dental plaques, dental caries, gingivitis (inflammation of gum tissues), and periodontal disease (destroy of tissue and bone).
Normal Microflora of Respiratory Tract:
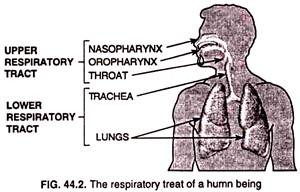
Respiratory tract (Fig. 44.2) is divided into the upper respiratory tract and the lower respiratory tract. The respiratory tract consists of nose and nasopharynx, oropharynx, and throat, while the lower respiratory tract consists of trachea, bronchi, and lungs.
1. Upper respiratory tract:
The normal microflora of the nose occurs just inside the nostrils, and consists of staphylococci, streptococci, Neisseria, Haemophilus, etc. Out of these S. aureus and S. spider-midis occur predominantly in approximately the same numbers as on the skin of the face.
The nasopharynx, the part of the pharynx lying above the level of the soft palate, usually contains small numbers of potentially pathogenic bacteria (e.g., Streptococcus pneumoniae, Haemophilus influenzae, Neisseria menengitidis. Diphtheroides occur commonly in both the nose and nasopharynx.
The oropharynx, the part of the pharynx lying between the soft palate and the upper edge of the epiglottis, contains streptococci (e.g. S. oralis, S. melleri, S. gordonii), large numbers of diphtheroids, Branhamella catarrhalis, and Neisseria menengitidis.
2. Lower respiratory tract:
The lower respiratory tract (trachea, bronchi, and lungs) has no resident microflora, despite the large numbers of microorganisms potentially able to reach this region during breathing. Dust particles, which are fairly large, settle out in the upper respiratory tract. As the air passes into the lower respiratory tract, the flow rate decreases markedly, and microorganisms settle onto the walls of the passages.
The walls of the entire respiratory tract arc lined with ciliated epithelium, and the cilia, beating upward, push bacteria and other particulate matter toward the upper respiratory tract where they are then expelled in the saliva and nasal secretions. Only particles smaller than about 10 μm in diameter reach the lungs.
Normal Microflora of the Gastrointestinal Tract:
Human gastrointestinal tract, the site of food digestion, consists of the stomach, small intestine, and large intestine. The composition of the gastrointestinal flora in humans varies considerably and is somewhat dependent on diet.
For convenience, humans who consume a considerable amount of meat show higher numbers of the highly proteolytic Bacteroides and lower numbers of coliforms and lactic acid bacteria than those who consume a vegetarian diet. Representative genera of microorganisms found in the gastrointestinal tract are shown in Fig. 44.3.
1. Stomach:
Many microorganisms are washed from mouth into the stomach but most of them are killed because the stomach fluids or gastric fluids are highly acidic (about pH 2-3). The stomach fluids therefore make the stomach a chemical barrier to entry of microorganisms into the intestinal tract.
As a result, the stomach usually contains less than to viable bacteria per millimeter of gastric fluids. The microorganisms present in stomach are mainly Helicobacter, Streptococcus, Staphylococcus, Lactobacillus, Peptostreptococcus, and yeasts (e.g., Candida). However, microorganisms such as Helicobater pylori may cause ulcers in susceptible human host.
2. Small intestine:
The small intestine is anatomically divided into three areas: the duodenum, jejunum, and ileum. The duodenum, adjacent to the stomach, is fairly acidic and contains few microorganisms (gram- positive cocci and bacilli bacteria) because of the combined influence of the acidic fluids of stomach and the inhibitory effect of bile and pancreatic secretions. Lactobacilly diphtheroids, Enterococcus faecalis, and Candida albicans (yeast) occasionally occur in the jejulum.
In ileum, the distal part of the small intestine, the pH becomes more alkaline and, as a result, anaerobic gram-negative bacteria and members of the family Enterobacteriaceae occur in it.
3. Large intestine:
The large intestine or colon contains the largest number of bacterial community in human body. The large intestine or colon acts as a fermentation vessel, and the microflora of it consists primarily of anaerobic, gram-negative, nonsporing bacteria and gram-positive, spore-forming, and nonsporing bacilli.
Facultative aerobes (e.g., Escherichia coli) are present but in smaller numbers in comparison to obligate anaerobes. The ratio of obligate anaerobes to facultative anaerobes is approximately 300 to 1. The total number of obligate anaerobes is large intestine is enormous; the counts of 1010-1011 cells/gram of intestinal contents are normal (bacteria constitute about one-third of the weight of faecal matter).
It is because the facultative aerobes consume oxygen making the environment of the large intestine strictly anaerobic. Besides bacteria, the yeast Candida albicans and certain protozoa (e.g., Entamoeba hartmanni, Trichomonas hominis, Endoliniax nana, lodamoeba sp.) may occur as commensals in large intestine.
4. Metabolic contributions of intestinal microflora:
Various essential metabolic reactions are carried out by intestinal microflora and, as a result, a variety of metabolic products are formed (Table 44.1).
Out of all vitamins produced in intestine, vitamin B12 and K are those essential vitamins that are not made by man rather by intestinal microflora and are absorbed therefrom. Steroids are produced in the liver and released into the intestine from gall bladder as bile acids.
Steroids are modified as active steroid compounds through different metabolic processes operated in the intestine by microflora, and absorbed therefrom. Gas (flatus) and odour-producing substances listed in the Table 44.1 are generated by the activities of fermentative bacteria and methanogens.
Normal human adults expel several hundred milliliters of gas from the intestines every day. Some foods metabolized by fermentative bacteria in the intestines result in the production of hydrogen (H2) and carbon dioxide (CO2). Methanogens occurring in the intestines of over one- third of normal human adults, convert H2 and CO2 produced by the fermentative microorganisms to methane (CH4).
Normal Microflora of the Urogenital (Genifourinary) Tract:
The uninary bladder itself is sterile in both male and female urogenital tracts, but the epithelial cells lining the urethra are colonized by gram-negative facultatively aerobic cocci and bacilli bacteria (e.g., Staphylococcus epidermidis, Enterococcus faecalis, Corynebacterium spp.). The genital tract (vaginal tract) of an adult female, because of its large surface area and mucous secretions, possesses complex microflora.
It is weakly acidic and contains significant amounts of the polysaccharide glycogen. Lactobacillus acidophilus (Fig. 44.4) ferments glycogen to produce lactic acid and maintains the acidic condition. Other microbes such as yeasts (Torulopsis and Candida species), streptococci, and E. coli may also be present. Vaginal microflora constantly changes between puberty and the menopause.
Before puberty, the female vagina is alkaline and does not produce glycogen, L. acidophilus is absent, and the flora consists predominantly of staphylococci, strepto-cocci, diphtheroids, and E. coli. After menopause, glycogen production ceases, the pH rise’s, and the flora again resembles that found before puberty.