The following points highlight the twelve main types of cells involved in immune responses. The types are: 1. Lymphoid Cells 2. T cells 3. B Cells 4. Natural Killer Cells 5. Mononuclear Phagocytes 6. Antigen-Presenting Cells 7. Polymorphonuclear Granulocytes and Plateletes 8. Basophils and Mast Cells 9. Platelets 10. Antigens 11. Haptens 12. Mediators of Immunity.
Type # 1. Lymphoid Cells:
Lymphoid cells differentiate from lymphoidal stem cells or common lymphoid progenitors present in the primary or central lymphoid organs. In mammals, the primary or central lymphoid organs are thymus gland (bilobed and located in the thorax, overlying the heart and major blood vessels), fetal liver and adult bone marrow cells.
Birds have a specialised primary lymphoid organ, the bursa of Fabricius, located in the dorsal wall of the cloaca. Lymphocytes are produced at a high rate (109 per day) from the lymphoid cells.
The lymphocytes which are produced in the thymus gland are called thymus derived lymphocytes or simply T cells or T lymphocytes. The lymphocytes which are produced in the bone marrow are called B cells or B lymphocytes.
In primary lymphoid organs, the nascent and virgin lymphocytes acquire their specific antigen receptors in order to cope with the threat of antigen. The cells are selected for tolerance to self-antigens and are capable of recognising only non-self antigens. This recognition is needed essentially in order to make an effective immune response.
Some of the lymphocytes migrate from primary lymphoid organs to secondary lymphoid organs via circulation. Secondary lymphoid organs include the spleen, lymph nodes and mucosa associated tissues including the tonsils and the Peyer’s patches of the gut.
Secondary lymphoid tissue provides an environment in which lymphocytes can interact with each other and with antigen. The average human adult has about 1012 lymphoid cells and the lymphoid tissue as a whole represents about 2% of the white blood cells. Many mature lymphoid cells are long- lived.
Type # 2. T cells:
T cells or T lymphocytes show a lot of variations in their morphology, function and the presence of markers or antigen binding receptors on their surface. On the basis of their variations, T lymphocytes have been classified variously. Morphologically, T lymphocytes are of two types which can be distinguished by light microscopy using Giemsa staining.
Two types of T lymphocytes are:
(a) Some T lymphocytes Eire smaller and non-granular [Fig. 21.6(a)] with a high N : C ratio (nuclear to cytoplasmic ratio). They also contain a cytoplasmic structure termed the Gall body which consists of a group of primary lysosomes associated with a lipid droplet.
(b) The large T lymphocytes have a lower N : C ratio and contain intracytoplasmic azurophilic granules [Fig. 21.6(b)], Recently these are called large granular lymphocytes (LGLS).
Functionally T lymphocytes come in several different types:
One group interacts with B lymphocytes and helps them to divide, differentiate and produce antibody.
Another group interacts with mononuclear phagocytes and helps them destroy pathogens.
These two groups of cells are T helper cells or TH-
(c) A third group of T cells is responsible for the destruction of host cells which have become infected by viruses or other intracellular pathogens—this kind of action is called cytotoxicity and these T cells are, hence, called T cytotoxic cells (Tc) or killer T cells (TK). Besides Tc cells several other cell types of the immune system also have some cytotoxic capacity, e.g., mononuclear phagocytes, macrophages, LGLs, eosinophil etc.
(d) Another type of T cell called suppressor T cell (Ts) also exists in the immune system. It is able to slow down or stop the activities of B cell and other T cell, playing a vital role in calling-off the attack when an infection has been conquered.
(e) Memory T cells (Tm) also generate during an initial infection. This defense cell may circulate in the blood or lymph for years, enabling the individual or body to respond more quickly to subsequent infection.
Lymphocytes express a large number of different molecules or markers on their surface which can be used to differentiate cell population. Many of these molecules have now been identified and a system of nomenclature has been developed and such system is referred to as CD system in which the molecules are numbered as CD1, CD2 etc.
The term CD (cluster of differentiation) refers to group or cluster of monoclonal antibodies, each cluster binding specifically to a particular cell-marker. However, the definitive T cell lineage marker is T cell antigen receptor (TCR).
There are two defined types of TCR—TCR1 and TCR2. Both receptors are associated with a set of five polypeptides, the CD3 complex to give the T cell receptor complex TCR-CD3 complex and express either TCR1 or TCR2.
Approximately 85% of blood T cells are TCR2 and the remaining 15% are TCR1. Both TCR1 and TCR2 can be divided into a number of subpopulations. T cell antigen receptors play A vital role in the immune system and regulate the effective response. The nature of the receptors on T cell mediates specific antigen recognition.
Type # 3. B Cells:
B cell is an important type of lymphocytes of the immune system. These cells are produced in the bone marrow. B cells [Fig. 21.6(c)] represent about 5-15% of the circulating lymphoid pool and are defined by the presence of surface immunoglobulin’s which act as cell surface antigen receptors.
Each B cell specifically recognises a particular antigen, using a receptor molecule on its surface. Having recognised as specific antigen, the B cells divide and differentiate with the help of T cell into either memory cell or antibody forming cell (AFCs) or plasma cells [Fig. 21.6(d)] which produce large amount of cytoplasmic immunoglobin molecules in a soluble form which can be secreted.
This is known as antibody. These antibody molecules are large glycoproteins found in the blood and tissue fluids, they bind to the antigen and inactivate them. The presence of antibodies also activates other part of immune system which, in turn, then eliminate the inactive antigen.
Type # 4. Natural Killer Cells:
These cells are mostly derived from the large granular lymphocytes. Most surface antigen of NK are shared with T cells or cells of the myelomonocytic series. NK cells are able to kill certain tumour cells and are also cytotoxic for virus infected cells.
NK cells may also release interferon-7 and other cytokines (immunological mediators) which may be important in the regulation of hemopoiesis and immune responses. NK cells have other important surface molecules which are common to all leucocytes. These surface molecules are important for cell adhesion and intercellular communication.
Type # 5. Mononuclear Phagocytes:
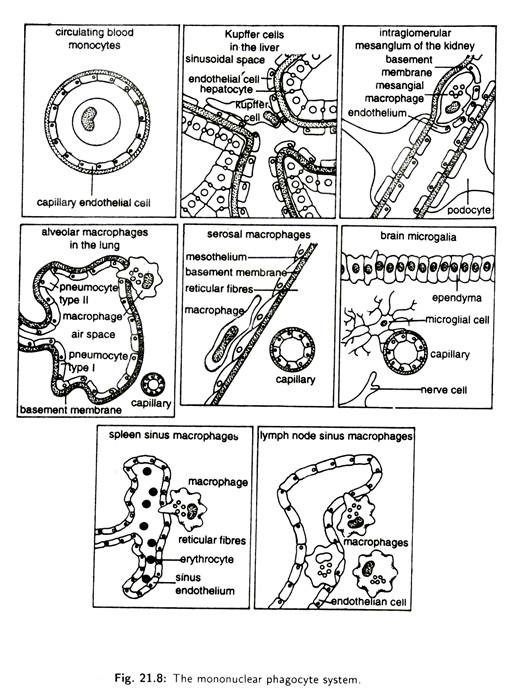
Hemopoietic stem cells of bone marrow or fetal liver give rise to mononuclear phagocyte system which is found is many organs [Fig. 21.7(a,b)]. Mononuclear phagocyte system includes the most important group of long-lived phagocytic cells.
The nucleus is never lobed and the cytoplasm is not granular and colourless. The main function of these cells is to engulf particles including infectious agents, internalize them and finally destroy them.
Hemopoietic stem cells differentiate into common myeloid progenitor which, ultimately, gives rise myeloid cells. The progenitor of the myeloid cell gives rise to pro-monocyte in the bone marrow. These differentiate into blood monocytes [Fig. 21.6(e).
They migrate through blood vessel into various organs where they become phagocytic cells which are called macrophages. But in blood, monocytes [Fig. 21.6(e)] are readily available than macrophages.
Macrophage or Monocyte possesses a well developed Golgi complex and many intracytoplasmic lysosomes. These lysosomes contain peroxidase and several acid hydrolases which are important in intracellular killing of microorganism.
Human monocyte or macrophage have mannosylfucosyl receptors (MFR) which bind to the sugars present on the surface of microorganisms. Monocytes or macrophages also have a receptor for lipopolysaccharide binding protein which is normally present in gram- negative bacteria.
The surface of monocyte or macrophages has many other receptors having different functions including phagocytosis, i.e., uptake of microorganisms.
Type # 6. Antigen-Presenting Cells:
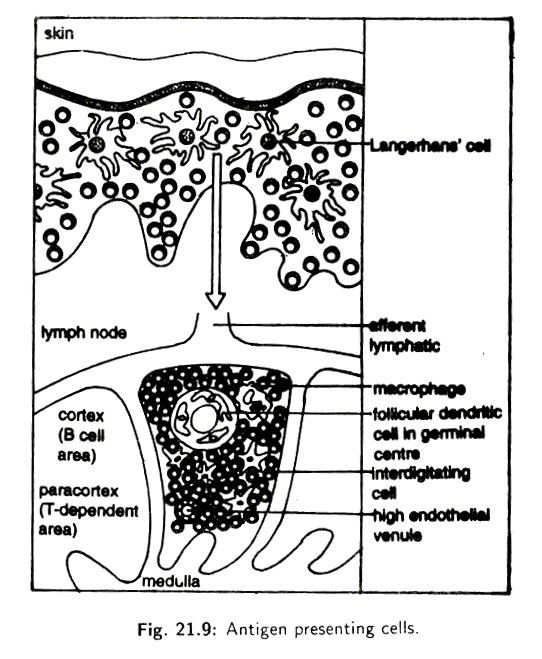
Antigen presenting cells (APCs) originate from the hemopoietic stem cells of bone marrow. In time they migrate out into the tissues as well as secondary lymphoid organs where the mature. APCs are primarily found in the skin, lymph node, thymus and spleen. APCs are heterogeneous population of cells such as Langerhans’ cell, dendritic cells, macrophages etc.
The prototypal APCs are the Langerhans’ cells which are found in the epidermis of skin. They move as veiled cells via lymphatic’s into the Para cortex region of lymph node. Within Para cortex the cells inter-digitate with many T cells (Fig. 21.8).
These interdigitating cells—localised in the T cell dependent areas of the lymph node, present antigen from the skin to the helper T- lymphocytes.
Other specialised APCs, the follicular dendritic cells, are found in the secondary follicles of the B cell and are as those in lymph node and spleen. They present antigen to the B cells.
APCs are also found abundantly in the thymic medulla (Fig. 21.9). APCS in the thymus are rich in self-antigen. The thymus is of crucial importance in the development and maturation of T cells. It appears that the interdigitating cells play a role in screening and detecting T cells that react against self- antigen. This process is known as negative selection.
Type # 7. Polymorphonuclear Granulocytes and Plateletes:
Most of the granulocytes are leucocytes whose cytoplasm is granular, containing specific chromophilic granules. The nucleus of the granulocytes is lobulated and contains 2-7 lobes. Due to presence of lobes in the nuclei these cells are called polymorph.
Granulocytes are formed within red bone marrow from myeloblasts at the rate of 80 million per minute and are short-lived (2-3 days). Granulocytes make up about 60-70% of the total normal blood leucocytes. They are also found to come out from blood capillaries to extravascular sites.
They can adhere to the endothelial cells lining the blood vessel and capillaries. When a pathogen enters into any part of body and secretes any toxin, leucocytes are stimulated by the toxin and they squeeze between them to escape from the blood vessel by chemo taxis to the extravascular infected sites.
This process is known as diapedesis. The adhesion is mediated by polymorph receptors and their ligand on the endothelial cells. Granulocytes are classified into neutrophils, eosinophil’s and basophils on the basis of their staining reaction with dyes.
Granulocytes do not show any specificity for antigen, but they play role in acute inflammation in protection against microorganisms. Secondly they also show phagocytic property.
Granulocytes are of following types:
(a) Neutrophils:
Neutrophils constitute over 90% of the circulating polymorphs and are 10-20 µm in diameter [Fig. 21.6(f)], Neutrophil contain a multi-lobed nucleus. It has a life span of only a few days and is incapable of division so that its supply must be continuously replenished by the bone marrow.
The cytoplasm of neutrophils possess two main types of granules—large primary granules and small secondary granules. The primary granules contain a variety of enzymes like hydrolases, myeloperoxidase and muramidase (lysosome). The secondary granules contain lysosome and lactoferrin.
The primary function of neutrophil is phagocytosis. When the bacteria invade the body and cause the inflammation, the neutrophil pass out of the blood vessels and surround the threatened area and, through their pseudopodia processes, engulf the bacteria and digest the bacteria and the dead tissue.
Due to this, the dead tissue in an inflammatory area becomes lignified and pus is formed. Extracellular release of granules and cytotoxic substances by neutrophils can also occur. Monocytes or macrophages also show the similar phagocytic properties but neutrophils are short lived cells which engulf material, destroy it and then die.
(b) Eosinophil:
Eosinophil’s comprise 2-5% of the blood leucocytes in healthy, non-allergic individuals and are 10-12 µm in diameter [Fig. 21.6(g)]. The cytoplasm of eosinophil contains coarse granules with central crystalloids. These granules in mature eosinophil’s are membrane-bound. The nucleus commonly possesses two to three lobes.
The eosinophil’s amoeboid but not phagocytic. Eosinophil’s play a very interesting and specialised role in immunity. By appropriate stimuli eosinophil’s are induced to release the content of granules to the outside of the cell. This process is known as degranulation. Degranulation involves fusion of the intracellular granules with plasma membrane.
The content of granules are released to the outside of the cell. This process is the only way that eosinophil’s can use their granule armament against large particle that cannot be phagocytosed. Eosinophil also releases histaminase and aryl sulphatase which inactive the action of histamine, the product of mast cells.
This effect reduces the inflammatory responses, allergy and slows down the migration of granulocytes into the site of invasion. When the number of eosinophil’s in blood goes down the normal count, a person may suffer from allergy like repeated attack of cough and cold.
Type # 8. Basophils and Mast Cells:
Basophils [Fig. 21.6(h)] are found in very small numbers in circulation, i.e., less than 0.2% of leucocytes. The cell diameter varies from 8 to 10 µm. The cell nucleus is lobed and kidney- shaped.
In this cell the cytoplasm contains large membrane-bound basophilic granules easily stained by basophilic dyes like methylene blue and hematoxylin. In a number of properties the basophil is identical to the group of connective tissue cells known as mast cells which are static and are not found in the circulation. That is why basophils are sometimes called circulating mast cells.
The static mast cells of connective tissue are large, round or oval in shape. The cells have nuclei either oval or round in form. The cytoplasm contains coarse granules. These cells play a role in the formation of the anticoagulant heparin, a vasoconstrictor serotonin and an allergy causing chemical histamine.
There are two different kinds of mast cells, the mucosal mast cell (MMC) associated with mucosal epithelia and the connective tissue mast cell (CTMC), MMCS are dependent on T cells for their proliferation whereas CTMCs are not dependent.
Basophils of blood also release heparin which prevents clotting of blood. Basophil in response to some stimulus releases histamine and these substances are released on degranulation. The stimulation for degranulation usually comes from an allergen, an antigen causing allergic reaction.
To be effective an allergen binds to the high affinity surface receptor of the mast cells or basophils. As a result, histamines are rapidly released by degranulation and cause the adverse symptoms of allergy which may also play a positive role in immunity.
Type # 9. Platelets:
Platelets [Fig. 21.6(i)] which are found only in mammalian blood are non-nucleated round or oval, biconvex discs having various sizes and covered by unit membrane. The platelets originate from large megakaryocytes cells found in the bone marrow and apparently are portions of cytoplasm of these cells which are pinched off and enter the circulation. The life span of platelets is 3-5 days.
It takes part in blood coagulation. In addition to their role in blood clotting, platelets are also involved in the immune responses specially in inflammation. Following injury to endothelial cells, platelets adhere to and aggregate at the endothelial surface of damaged vascular tissue. They release substances that increase permeability and release factors that activate complement and hence attract leucocytes.
Type # 10. Antigens:
The immune system has the capacity to distinguish between self and non-self through an elaborate recognition process. Prior to birth the body somehow makes a large directory of the body (or self) proteins and large molecules. Subsequently these molecules can be distinguished from non-self ones and the body can successfully react immunologically against the non-self molecules.
Non-self foreign substances such as proteins, nucleoproteins, polysaccharide, virus, pollen grain, fungal spore, some glycolipids etc.—to which the immune system responses and produces specific antibody—are termed antigens or antibody generators or immunogens.
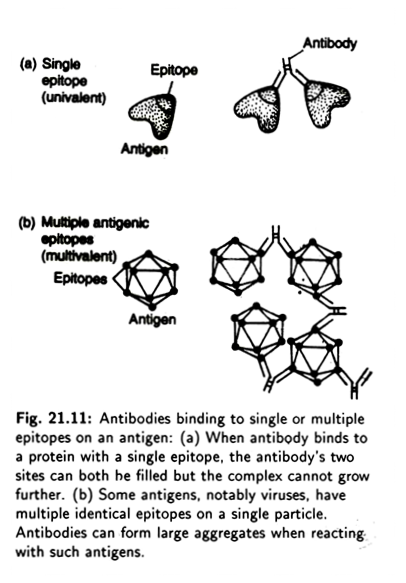
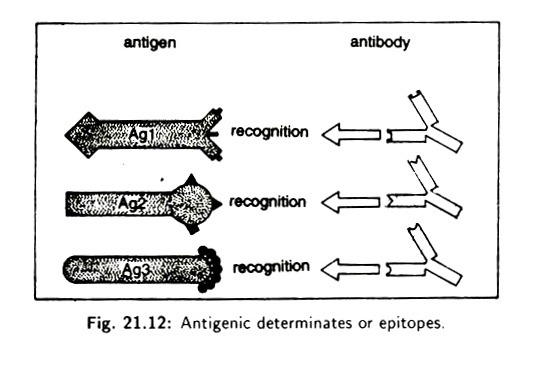
Antigens are large complex molecules with molecular weight more than 10,000. Nonetheless, all macromolecules do not behave as antigens. Antigen molecules each have an antigenic determinant, also called epitopes (Fig. 21.10).
An antigen may possess several epitopes. The number of epitopes on an antigen is termed as its valence. Thus, antigens may become univalent, bivalent or multivalent (Fig. 21.11). Multivalent antigens generate greater antigen immune response.
The epitopes on one antigen (Ag1 in Fig. 21.11) are usually different from those on another (Ag2 in Fig. 21.11). Some antigens (Ag3 in Fig. 21.11) have repeated epitops. Epitopes are molecular shaped recognised by the antibodies and T cells receptors of the adaptive immune system. Each antibody receptor recognises one epitope rather than the whole antigen. Even simple microorganisms have many different antigens.
Hence there may be several different antibodies for a given microorganism, each binding to a different antigen on that microorganism’s surface. T cell also recognize antigens but they recognize antigens originating from within cells, small polypeptide fragments which are presented at the surface of other host cells.
For example, a host cell which has been infected with a virus will express small fragments of viral proteins on its surface, thus making it instantly recognizable by Tc cells.
The antigen fragments are presented on the surface of the cell by a specialised group of molecules. These are encoded in a set of genes known as the Major Histocompatibility Complex (MHC) and are consequently called MHC molecules. The T cells use their antigen-specific receptors (TCRS) to recognize the antigen peptides bound to these MHC molecules.
Type # 11. Haptens:
Many small organic molecules are not antigenic by themselves but may become so if they bind to a large carrier molecule such as protein. These cannot stimulate antibody formation by themselves but they react with antibodies once formed.
Such small molecules are termed as haptens. For example, penicillin by itself is not antigenic. However, when it combines with serum proteins of sensitive individuals, the resultant molecule initiates a severe immune reaction, manifested as allergy. Here the hapten is acting as an epitope for the carrier protein.
Type # 12. Mediators of Immunity:
There are a variety of molecules in the development of immune responses. These include antibodies or immunoglobulin’s and cytokines produced by lymphocytes complement proteins of serum and a group of protein molecules which are normally present in serum. The concentration of these proteins increases rapidly during infection and they are, therefore, called acute phase proteins.
They are important in the innate immunity to infection. These proteins in presence of Ca++ recognise and bind to the molecular group found on a wide variety of bacteria and fungi.
When they bind to bacteria, they promote the binding of complement protein which stimulates phagocytes to engulf the bacteria (Fig. 21.12). This process of protein- coating to enhance phagocytosis is known as Opsonisation. Both acute phase proteins and complement proteins are called opsonins.