Let us make an in-depth study of the blood sugar level. After reading this article you will learn about: 1. Regulation of Blood Sugar Level 2. Role of Blood Sugar as an Aid to Diagnosis 3. Normal Blood Glucose Level under Various Nutritional States 4. Abnormalities in the Regulation of Blood Sugar Level and 5. Conditions in which Blood Glucose Estimation is Carried Out for Diagnosis.
Contents
Regulation of Blood Sugar Level:
Blood Glucose Hemostasis:
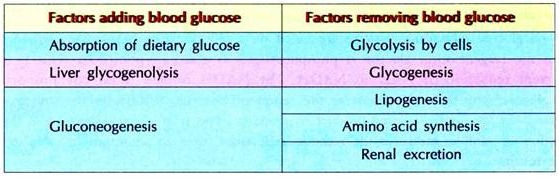
After a meal, specially, rich in carbohydrates, the intestine adds glucose to the blood by absorption and this leads to an increase in the blood glucose level from 60-90 mg/100 ml to 100-140 mg/100 ml. A further increase in blood glucose is prevented mainly by the liver, which takes up most of the dietary glucose and stores it as glycogen by glycogenesis.
Simultaneously, a hormone i.e. insulin, is released by the β-cells of islets of Langerhans of the pancreas. This hormone helps in the uptake of glucose by other tissues, and thereby all the tissues start utilizing glucose as the primary metabolite for the production of energy by glycolysis. In each and every tissue, a small amount of glucose is stored as glycogen.
Muscle stores much of glucose as muscle glycogen. When the storage of glucose saturates the liver, muscle and other tissues, then the adipose tissue convert the excess of glucose to fat by lipogenesis and store as triacylglycerol’s (TAG). Fats are also synthesized by the liver from excess of glucose and amino acids. Insulin aids in the entry of glucose in almost all the cells of the tissues of the body except five tissues viz., liver, brain, intestine, RBC and retina of the eye (hence causes cataract in diabetes mellitus patients).
If the glucose level in the blood increases further, more than 180 mg/100 ml (hyperglycemia) as occurs in intravenous injection of glucose or due to incapability of the cells to utilize glucose absorbed in normal amounts (insulin deficiency, defective insulin receptors or more of insulin antagonists i.e. diabetes mellitus, see details later in this article), then the kidney starts excreting glucose, a condition known as glucosuria.
Glucosuria occurs when the capacity of the kidney to tolerate blood glucose is exceeded in the blood. This is known as renal threshold for glucose, the value for which is 180 mg/100 ml of blood. If the glucose concentration in the blood exceeds this value, it is excreted in urine. At 180 mg/100 ml of blood glucose the kidney reabsorbs 350 mg of glucose per minute, this is known as tubular maximum for glucose (T-G). Any amount of glucose being filtered by the glomerular filtrate more than this into the kidney per minute is excreted.
When the blood glucose level starts falling (hypoglycemia), as seen in fasting, starvation, shock, severe exercise, febrile disease, lactation, multiple pregnancies etc., the hormone glucagon is released by the α-cells of islets of Langerhans of the pancreas. Glucagon stimulates the breakdown of glycogen in the liver (glycogenolysis) by activating liver phosphorylase.
In conditions of shock and emotional excitement, epinephrine is released from the adrenal medulla which stimulates glycogenolysis in muscle by activating muscle phosphorylase. The maximum reserves of liver glycogen can maintain the blood glucose level within the normal range for 8-10 hours of fasting. After this, liver produces glucose by gluconeogenesis from lactate derived from muscle or RBC glycolysis and amino acids derived from muscle proteins.
The extent to which gluconeogenesis can provide glucose to the blood depends upon the muscle mass and the rate of glucose utilization, which in turn depends upon the fat content of the body. In normal healthy adult, gluconeogenesis can maintain blood glucose for about 30-40 days of starvation. After which severe hypoglycemia and death occurs. In addition to liver, kidney can also take part in gluconeogenesis. The hormones which facilitate gluconeogenesis are glucocorticoids, GH, ACTH, and thyroid hormones.
Role of Blood Sugar as an Aid to Diagnosis:
The major sugar present in the blood is Glucose.
There are three methods by which glucose in the blood can be measured viz.:
(1) Enzymatic method
(2) Complex formation and
(3) Reduction method.
1. Enzymatic Method:
The enzyme, glucose oxidase is used in the estimation of blood glucose. Glucose oxidase oxidizes glucose to gluconic acid, releasing hydrogen peroxide. Hydrogen peroxide then reacts with an oxygen acceptor, such as orthodianisidine, phenylamine-phenazone or any other chromogenic oxygen acceptor with the help of the enzyme peroxidase. The intensity of the color developed is directly proportional to the blood glucose level. This enzyme is very specific for glucose, hence the value obtained is true glucose value in the blood.
2. Complex Formation:
The carbonyl carbon is reacted with reagents like ortho-toluidine to form a coloured complex. The intensity of the colour developed is proportional to the carbonyl compounds present in the blood. Hence the value obtained is not a true glucose value; it is the value for all the carbonyl compounds present in the blood like glucose, fructose, galactose, and ribose. Since ortho-toluidine is carcinogenic, this method is discouraged.
3. Reduction Method:
This is based upon the reducing property of glucose. Due to the presence of free aldehyde group glucose easily reduces metal ions like copper, iron, bismuth. The reduced ions are then reacted with a colouring agent; the intensity of the colour developed is proportional to the amount of reducing substance present in the blood.
There are many other reducing substances other than glucose present in the blood like:
fructose, lactose, mannose, ribose, ascorbic acid (vitamin C) etc. Hence the values obtained are far from the actual amount of glucose in the blood. But this method is relatively economical; hence most of the diagnostic laboratories adopt this method (Folin-Wu-method) for the estimation of blood glucose.
Modern Electronic Gadgets for Estimation of Blood Glucose:
Most of them are based on a glucose oxidase-colorimetric reaction that occurs when a drop of blood is placed on a reagent—impregnated pad. The test pad contains the enzyme glucose oxidase, peroxidase, and color indicators. When whole blood is placed on the test pad, glucose is oxidized to gluconic acid and hydrogen peroxide with glucose oxidase acting as a catalyst. The hydrogen peroxide then oxidizes an oxygen acceptor in the presence of peroxidase to form a color change, the intensity of which is directly proportional to the amount of glucose in the blood sample.
A reflectance photometer or an amperometric system is used to measure the reaction that takes place on the reagent strip. Hence, the reagent strip is inserted into the test chamber. When light shines on the reagent pad, light is reflected. This reflected light is measured electronically and a blood glucose concentration value is displayed.
Other systems use electrochemical methodologies. These monitors quantify glucose amperometrically by measuring the current that is produced when glucose oxidase catalyses the oxidation of glucose to gluconic acid or when glucose dehydrogenase catalyses the oxidation of glucose to gluconolactone.
The electrons generated during this reaction are transferred from the blood to the electrodes. The magnitude of the resultant current is proportional to the concentration of glucose in the specimen and is converted to a readout displayed on the monitor.
Some blood glucose monitoring systems are based on a reflect metric hexokinase method. When blood is applied to the reagent strip, glucose is phosphorylated to glucose-6-phosphate. This is later oxidized with concurrent reduction of NAD to NADH. The NADH formed is directly proportional to the amount of glucose (any hexose) present in the sample.
Then the NADH, in the presence of another enzyme, reduces the dye and a colored product is generated. The strip which is inserted in the photometer after application of sample, measures the reaction reflectance, uses an algorithm to calculate glucose and displays the result.
Normal Blood Glucose Level under Various Nutritional States:
1. Fasting or post-absorptive state:
(i.e. 12-14 hours after a meal) ranges between 60-90 mg/100 ml of blood (true blood glucose, but by reduction methods it is 80-120 mg/100 ml).
2. Post-prandial:
That is after meals (1-2 hours after the first meal) blood glucose level ranges between 100-140 mg/100 ml (or 5.5-8.0 mmols/L and 3.3-5.0 mmols/L, fasting state).
3. Random blood glucose level:
It is measured any time after 1st, 2nd or 3rd meal that ranges between 100-180 mg/100 ml (or 5.5-10 mmols/L). The level of glucose in the blood is maintained by various mechanisms of the body. The purpose of regulation of the blood glucose levels within the normal physiological limits is that, if the blood glucose level falls below 60-20 mg/100 ml, a condition known as hypoglycemia occurs.
Hypoglycemia results in convulsions leading to profuse sweating, weakness, tremors, fainting, coma and finally death. All these conditions observed in hypoglycemia are due to insufficient supply of glucose to the brain, as brain uses glucose only as the source of energy and not any other substance.
When the blood glucose level rises above 180-360 mg/100 ml (a condition known as hyperglycemia) then it results in—
1. The excretion of glucose by the kidney, due to which the work load on the kidney increases, leading to kidney disorders and finally to kidney failure.
2. Due to the high concentration of glucose, the oncotic pressure (osmotic pressure of plasma) differs leading to unequal distribution of water and electrolytes.
3. Increased glucose concentration in the blood for a longer duration of time leads to various infections, as the microorganisms can grow easily. Delay in wound healing and post surgical recovery, are the other problems encountered due to excessive microorganism growth in hyperglycemia.
4. High blood glucose level leads to glycosylation of proteins of the blood vessels and capillaries, resulting in narrowing of the passage of the flow of blood (increases the blood pressure). Continuous glycosylation of the proteins disrupts the membranes and results in accumulation of blood clots and cholesterol, a condition known as atherosclerosis of arteriosclerosis. Glycosylation of the membranes also leads to reduced life of RBC, cell necrosis, kidney failure etc.
Abnormalities in the Regulation of Blood Sugar Level:
Diabetes Mellitus:
Frequent urination tasting sweet.
It is a condition wherein the cells are incapable of utilizing glucose, due to which the blood glucose level increases (hyperglycemia) and subsequently, there is an increased excretion of glucose in the urine (glycosuria) and hence the urine tastes sweet.
Causes:
1. Deficiency of insulin (Insulin Dependent Diabetes Mellitus—IDDM—i.e. type-I diabetes).
2. Excess of insulin antagonists like glucagon, epinephrine, GH etc.
3. Defective or absence of insulin receptors on the cells (Insulin Independent Diabetes Mellitus- IIDM—i.e. type-II diabetes).
Biochemical Changes in Diabetes Mellitus:
When the cells are incapable of utilizing glucose for energy production, they start utilizing amino acids and fats for the production of energy. There will be production of ketone bodies by the liver and if they are produced in excess it causes accumulation of ketone bodies in the blood (ketonemia) and subsequent excretion in the urine (ketonuria).
Both the conditions together lead to diabetic ketosis. Due to this the pH of plasma is lowered. The excretion of glucose and ketone bodies requires large amounts of ions and water leading to polyuria and weight loss.
Hence the three main conditions seen in diabetes mellitus are:
1. Polyuria:
Frequent urination leading to dehydration.
2. Polydypsia:
Frequent intake of water due to frequent urinadon.
3. Polyphagia:
Frequent intake of food due the starving condition of the cells.
Classification of Diabetes Mellitus:
1. Juvenile or Hereditary:
Onset of diabetes mellitus in childhood is known as juvenile type. Here there is a defect in the gene synthesizing insulin or its receptors which is an inborn and hereditary character.
2. Maturity onset type:
After maturity due to obesity or decrease in the function of the gene or due to other reasons, the insulin is not produced in normal amounts or if produced in normal amounts, cannot act on the target cells.
3. Secondary diabetes:
Due to excess of insulin antagonists.
Detection and Screening of Diabetes Mellitus:
1. Benedict’s reducing sugar test:
This is the preliminary method for the detection, of diabetes mellitus. Reducing sugars i.e. glucose in urine reduces copper to form a precipitate which depends upon the concentration of glucose. If 0.5% of glucose is present in urine, it forms a green coloured precipitate, 1.0% → yellow, 1.5% → orange, → 2.0% → brick red precipitate.
Benedict’s test is an easy and simple test to perform. Hence, at the first instance, detection of diabetes mellitus is done with urine sugar. If Benedict’s test is positive then estimation of blood sugar is taken up. Further if blood glucose level is higher than the normal then diabetes mellitus is confirmed by the following tests.
2. Glucose tolerance test (GTT):
Glucose tolerance test is done in patients, suspected with diabetes mellitus, but does not show any glucosuria because some persons have a very high renal threshold for glucose i.e. 250-300 mg/100ml. Secondly GTT is carried in those suspected diabetes mellitus cases whose blood glucose level shows around the normal values i.e. fasting blood glucose is less than 90 mg/100 ml but more than 60-70 mg/100 ml.
Glucose tolerance test is done with the patient being kept on a carbohydrate rich diet i.e. more than 150 gm./day, for three days prior to the experiment. The blood glucose is measured in fasting condition (12-14 hours).
Then he is given an oral dose of 50-60 grams of glucose in 300 ml of water (i.e. 0.75 grams per kg body weight for Indian adult male or 1.0 gm/kg body weight for individuals of developed countries). Blood glucose is estimated every half an hour after ingestion of glucose and the ability of the individual to tolerate glucose is assessed, which gives an idea of diabetes mellitus.
The result of glucose tolerance is plotted in a graph as follows:
Graph—A:
In normal persons the fasting blood glucose level will be at the lower limit i.e., 75 mg/ 100 ml. Upon providing oral glucose the blood glucose rises in one hour’s time and falls below the fasting level in another half to one hour due to the secretion of insulin. Then, in about a time of 7th hours it reaches back to normal. Such a person is normal and can tolerate glucose and is not a diabetic patient.
Graph—B:
In diabetes the fasting blood glucose may be within the normal range but when glucose is given orally, there will a steep rise in blood glucose in ½ an hour and it increases further till one hour and it does not come down to normal level even by 2½ hours. Such patients are said to be intolerant to glucose and hence are diabetes mellitus patients.
If GTT is positive i.e. if the patient is a confirmed diabetes mellitus patient then further investigations are required to trace out the type of diabetes i.e. insulin dependent or independent. This can be done by performing (1) Insulin Tolerance Test (ITT) and (2) Glucagon Tolerance Test (GuTT).
Insulin Tolerance Test:
Insulin is a hormone which is secreted by the P-cells present in islets of Langerhans, of pancreas. It helps in the uptake of glucose by the cells. Insulin tolerance test is done with the patient being kept on a carbohydrate rich diet i.e. more than 150 gm/day for three days prior to the experiment.
His blood glucose is measured in fasting condition (12-14 hours). Then he is given intravenous dose of 0.1 unit of insulin/kg body weight. Blood glucose is estimated every half an hour after injection of insulin and the ability of the individual to tolerate insulin is assessed, which shows whether the diabetes mellitus can be treated with insulin or not i.e. is it insulin responsive (IDDM) or not.
The result of insulin tolerance is plotted in a graph as follows:
Graph—A:
Injection of insulin in normal persons or insulin responsive diabetes mellitus (IDDM) persons will lead to a fall in the blood glucose level in one hour’s time due to utilization of glucose by the cells aided by insulin and slowly increases and rises above the fasting level (base line) in another half to one hour due to the secretion of glucagon.
Then in about the time of 2½ hours it reaches back to normal. Such a person is normal and can tolerate insulin. If the person is a confirmed diabetes mellitus case then it is insulin responsive diabetes mellitus or insulin dependent diabetes mellitus (IDDM).
Graph—B:
In insulin non responsive diabetes mellitus patients there will not be any decrease in the blood glucose level or the decrease will be very marginal upon injection of insulin. This may be either due to excessive insulin antagonists or defective insulin receptors on the cell membrane (may also be due to antibodies to insulin-natural or injected one).
Glucagon Tolerance Test:
Glucagon is a hormone that is secreted by the a-cells of islets of Langerhans of pancreas which helps in the release of glucose from the cells. Glucagon tolerance test is done with the patient being kept on a carbohydrate rich diet i.e. more than 150 gm./day for three days prior to the experiment.
The blood glucose is measured in fasting condition (12-14 hours) and then the patient is given intravenous dose of 30 µg of glucagon/kg body weight. Blood glucose is estimated every half an hour after injection of glucagon and the ability of the individual to tolerate glucagon is assessed, which shows whether the diabetes mellitus is due to excessive insulin antagonists or not.
The result of glucagon tolerance is plotted in a graph as follows:
Graph—A:
Injection of glucagon in normal persons or insulin non-responsive diabetes mellitus persons will lead to increase in the blood glucose level in one hour’s time due to release of glucose from the cells by the action of injected glucagon and slowly decreases and falls below the base line in another half to one hour due to cessation of the action of injected glucagon (upon degradation) or in normal non-diabetic persons there will be secretion and action of insulin.
Then in about the time of 2½ hours it reaches back to normal. Such a person is normal and can tolerate glucagon. If the person is a confirmed insulin independent diabetes mellitus case, then it can hereby be confirmed that the person is not responding to insulin not because of excessive insulin antagonists but may be due to defective insulin receptors on the cell membrane or antibodies to insulin.
Graph—B:
In diabetes mellitus patients with excessive insulin antagonists this type of graph is obtained wherein, there will not be any increase in the blood glucose level or the increase will be very marginal upon injection of glucagon. Thus it can be confirmed that the diabetes mellitus is due to excessive insulin antagonists like glucagon’s, growth hormone, epinephrine, glucocorticoids, testosterone (all the hormones except insulin are insulin antagonists).
Hemoglobin A1c:
It is the main fraction of glycosylated hemoglobin (glycohemoglobin) that is the hemoglobin to which glucose is bound. Hemoglobin A1c is tested to monitor the long-term control of diabetes mellitus.
The level of hemoglobin A1c is increased in the red blood cells of persons with poorly controlled diabetes mellitus. Since the glucose stays attached to hemoglobin for the life of the red blood cell (normally about 120 days), the level of hemoglobin A1c reflects the average blood glucose level over the past 4 months. The normal level for hemoglobin A1c is less than 7%.
Diabetics rarely achieve such levels, but tight control aims to come close to it. Levels above 9% show poor control, and levels above 12% show very poor control. It is commonly recommended that hemoglobin A1c be measured every 3 to 6 months in diabetes. Diabetics who keep their hemoglobin A1c levels close to 7% have a much better chance of delaying or preventing diabetes complications that affect the eyes, kidneys, and nerves than people with levels 8% or higher.
A change in treatment is almost always needed if the level is over 8%. Lowering the level of hemoglobin A1c by any amount improves a person’s chances of staying healthy.
A 1% change in an A1c result reflects a change of about 30 mg/dl (1.67 mmol/L) in average blood glucose. For instance, an Ale of 6% corresponds to an average glucose of 135 mg/dl (7.5 mmol/L), while an A1c of 9% corresponds to an average glucose of 240 mg/dL (13.5 mmol/L).
Estimation:
About 90% of hemoglobin is hemoglobin A, approximately 8% of hemoglobin A is made up of minor components that are chemically slightly different. These minor components include hemoglobin Ale, Alb, Alal, and Ala2. Hemoglobin Ale (HbA1c) is a minor component of hemoglobin to which glucose is bound.
HbA1c also referred to as glycosylated or glucosylated hemoglobin has a chemical (electrical) charge on the molecule and the amount of the charge differs from the charges on the other components of hemoglobin. The molecule of HbA1c also differs in size from the other components. HbA1c may be separated by charge and size from the other hemoglobin A components in blood by a procedure called high pressure (or performance) liquid chromatography (HPLC).
HPLC separates mixtures (e.g. blood) into its various components by adding the mixtures to special liquids and passing them under pressure through columns filled with a material that separates the mixture into its different component molecules. Because HbA1c is not affected by short-term fluctuations in blood glucose concentrations, for example, due to meals, blood can be drawn for HbA1c testing without regard to when food was eaten.
Since HbA1c is not influenced by daily fluctuations in blood glucose concentration, it cannot be used to monitor day-to-day blood glucose concentrations and to adjust insulin doses nor can it detect the day-to-day presence or absence of hyperglycemia or hypoglycemia.
HbA1c may be increased falsely in certain medical conditions. These conditions include uremia (kidney failure), chronic excessive alcohol intake and hypertriglyceridemia. Medical conditions that may falsely decrease HbA1c include acute or chronic blood loss, sickle cell disease or thalassemia. Diabetes during pregnancy, commonly referred to as gestational diabetes, may falsely increase or decrease HbA1c.
Conditions in which Blood Glucose Estimation is Carried Out for Diagnosis:
1. Blood glucose is estimated in order to diagnose diabetes mellitus, wherein hyperglycemia is observed.
2. While conducting glucose tolerance test for confirmation of diabetes mellitus—wherein hyperglycemia is observed.
3. While conducting insulin tolerance test in order to confirm the type of diabetes—hypoglycemia is seen relative to 0 hour in Insulin Dependent Diabetes Mellitus (IDDM) cases.
4. While conducting glucagon tolerance test to detect the type of diabetes—if hyperglycemia is seen it indicates that diabetes is due to defective insulin receptors and if there is no change in the blood glucose level, it indicates that the diabetes is due to excessive insulin antagonists.
5. Diagnosis of hypoinsulinism due to defective pancreas—wherein hyperglycemia is seen.
6. Detection of hyperinsulinism due to pancreatic tumours—wherein hypoglycemia is seen.
7. To assess glycogen storage diseases due to defective enzymes of glycogen metabolism in the liver— hypoglycemia is seen.
8. While performing epinephrine tolerance test—hyperglycemia is seen. If hypoglycemia is exhibited it indicates glycogen storage diseases.
9. During oral leucine administration test—hypoglycemia is seen, since leucine taken orally enhances insulin production.
10. During insulin therapy—hypoglycemia occurs. If hypoglycemia is very severe and persists for longer period, then it indicates that the insulin dose for treatment of diabetes mellitus is more than required and it has to be reduced.
11. Detection of excessive insulin antagonists—hyperglycemia.
12. During renal dysfunction hypoglycemia is seen due to non-reabsorption of filtered glucose by the kidney tubules. In total renal failure there is relatively hyperglycemia because glucose is neither filtered nor excreted.
13. In the assessment of hypocalcaemia blood glucose estimation can be done, wherein there will be hyperglycemia because insulin cannot be released in absence of Ca and Zn from the islets of Langerhans of pancreas.
14. To assess the intestinal status of carbohydrates, rich carbohydrate diet creates hyperglycemia and poor carbohydrate diet creates relative hypoglycemia.
15. Post exercise blood glucose level will be more i.e., hyperglycemia. In regular athletes there will be relative hypoglycemia.