The following points highlight the three types of human beings classified depending on energy requirement. They are: 1. Sedentary People 2. People with Moderate Work and 3. Heavy Workers.
Human beings are classified into 3 groups depending on the energy requirement.
1. Sedentary People:
Require less calories of energy i.e. up to 2400 Kcal/day.
2. People with Moderate Work:
Require about 2800 Kcal/day.
3. Heavy Workers:
Require about 3000 Kcal/day.
Pregnant and lactating mothers require additional 800 and 700 Kcal/day respectively.
Calculation of total calorie requirements and building a balanced diet:
A moderate medical student requires 2800 Kcal of energy/day—how to calculate it?
Weight of the person → 55 kg
Height of the person → 162 cms
Surface area of the person → 1.55 sq.m
BMR → 41 cal/sq m/hr
Basal energy required → BMR x surface area x 24 hrs. 41 x 1.55 x 24 = 1525 cal
Specific dynamic action (SDA) → 10% of basal energy requirement = 152.5 Cal
If a moderate medical student does 8 hours of moderate work (add 100 cal/hr.)
8 hours of sedentary work → = 320 cal
(add 40 cal/hr.)
Total basal energy → 1525 + 800 + 320 = 2645
Total calorie requirement → 2645 + 152.5 = 2797.5 ~ 2800 Kcal
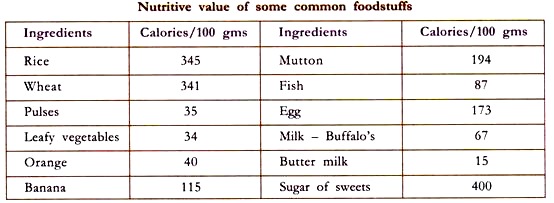
Balanced diet for a vegetarian moderate medical student with a total calorie requirement of 2800 Kcal/ day as worked out by Indian Council of Medical Research (ICMR).
Effect of pregnancy:
A pregnant mother requires additional energy to maintain the metabolism of the foetus, build up a reserve of fat and additional maternal tissue. By the end of a pregnancy the mother gains approximately 1 kg protein, mostly in the uterus and products of conception and 4 kg of fat in her own fat depots.
Energy will be required for the metabolism of the foetus and placenta, metabolism of additional uterine and breast tissues and for the extra work of heart and respiration. An extra amount of about 70,000 Kcal spread evenly at an almost constant rate over the last 2/3rds of pregnancy is generally required. An average woman at rest thus will need approximately 300-400 Kcal/day.
During the last stages of pregnancy approximately 60 litres/day of extra oxygen, equalling approximately 300 Kcal, is consumed. If the mother continues her normal activities these are certain to cost her more than before pregnancy on account of the increase in her weight. Specific nutrient requirements are less easy to specify. The need for proteins is greatest in the last 10 weeks when it accumulates at a rate of 5-6 g/day.
Lactation:
A lactating mother must also consume extra food to meet the energy cost of lactation. The efficiency of milk production is probably 80%, so that for the production of milk having an energy value of 80 Kcal, the mother must expend 100 Kcal, thus requiring the same amount of energy in her diet. A healthy baby may require 850 ml of milk daily.
At an energy value of 68 Kcal/100 ml of milk, this will mean making the provision of 578 Kcal/day. A lactating mother will thus require an extra diet of approximately 720 Kcal/day to meet the demands of lactation. However, the fat reserves which are carefully laid down during pregnancy are also handy for this energy requirement.
Metabolic changes in starvation:
Fasting is a post absorptive state probably after 12-14 hours after the last meal. Starvation commences thereafter, during which the liver glycogen is broken down and falls to about 10% of its normal concentration and remains at that level almost during the entire remaining period of starvation.
The blood glucose level remains at 80 mg/100 ml, increased mobilization of depot fats occurs. The ketone bodies level increases leading to ketoacidosis. The pH of the blood decreases due to decrease in bicarbonate. The R.Q comes from 0.82 to 0.70. Within a few days the excretion of urinary nitrogen increases, due to the increased breakdown of the protein even though adequate fat stores are available.
This is to supply glucose to the brain by gluconeogenesis. The earliest proteins to be depleted are the enzymes of G.I tract, then the hepatic enzymes are involved and finally muscle starts loosing the proteins. In the starting about 100 grams of proteins are metabolized, by 4-6 weeks it falls to 12-15 grams per day because the brain develops the ability to utilize the ketone bodies i.e. beta hydroxybutyric acid. Once the fat stores are depleted the condition of the fasting person takes a rapid turn to worse.
Absence of food does not affect the normal functioning instead is helpful in the treatment of certain disorder of G.I. tract, diabetes mellitus and obesity. Protein calorie malnutrition or protein energy malnutrition: When there is insufficient supply of dietary proteins, all the cells lack amino acids for their synthetic activities and growth slows down or stops. The earliest feature of protein deficiency is indigestion and failure of absorption of food, because of lack of synthesis of digestive enzymes. As a result chronic diarrhea sets in. The liver cells fail to synthesize plasma albumin and this leads to water retention and oedema.
Skeletal muscles and RBC fail to maintain their structure and functions resulting in wasting of muscles and anemia. These clinical conditions comprise a spectrum of disease in early childhood and are collectively known as protein energy malnutrition. The diseases are marasmus and kwashiorkor.
Marasmus:
It is a disease caused if the child is not fed a little extra over the mother’s milk from the fourth month after birth. If the child is fed only on mother’s milk for 18 months then it results in calorie malnutrition leading to marasmus. Marasmus also occurs if the child is fed with highly diluted bottle milk which lacks calories. It is also seen in the areas of famine and in children of poor families.
The marasmic child looks very weak and thin. Hands and legs look like sticks. Head looks big and old. Muscles are weak with hypoproteinemia. The infant fed on a diet low in both protein and calories become undernourished and lose weight considerably with chronic diarrhea. If it is not corrected it leads to extreme wasting of subcutaneous fat and muscles. There is no oedema in marasmus.
Kwashiorkor:
This condition is mostly seen at the age of 14 months due to protein deficiency. It is a disease caused due to ‘weaning away the child from mothers milk’, most probably to give way to the second child. Now the child is bottle fed or he will be fed with other foods which cannot supply the proteins required for the growth of the child. This results in the deficiency of proteins in the child (protein malnutrition).
Due to the poor quality of the proteins in the diet the amino acids are not utilized for protein synthesis, instead are converted into fats, therefore there is a net increase in calories in the body which is stored as fats due to which the body of the infant becomes fat and rounded. The hands and the legs will be swollen due to the presence of large amounts of water (oedema).
The muscles become thin and weak. The skin becomes pale and starts peeling off the body. Hairs become loose and come out easily on pulling. The biochemical changes occurring during kwashiorkor are hypoproteinemia, especially hypoalbuminemia, due to which oedema occurs (unequal distribution of water between the tissue and body fluids). The other effects are anemia, fatty livers, hepatic cirrhosis, muscle wasting etc.
The chief characteristics of kwashiorkor are:
(a) Lack of appropriate cellular development.
(b) Oedema.
(c) Diarrhea.
(d) Poor growth.
(e) Low plasma protein level.
(f) Muscle wasting.
(g) Increased susceptibility to infection.