The following points highlight the three main types of genetic mechanisms. The types are: 1. Immuno-Genetics 2. The HLA System 3. The Rh Factor.
Type # 1. Immuno-Genetics:
Genetic mechanisms which control immune responses have opened up an entire new field of immuno-genetics. Basically it is the study of antigens, antibodies and their reactions. An antigen is a substance present in the body or introduced from outside which can initiate an immune reaction.
The antigens present on the surface of red and white blood cells are important in immuno-genetics. The immune reactions in response to the antigen take place in the lymphoid organs (spleen, lymph nodes and tonsils) and result in the production of antibodies or sensitized lymphocytes which are effective in eliminating the antigen from the body. As there are millions of potential antigens, there are many millions of species of antibody molecules that are synthesised by the immune system.
Antibodies are serum proteins belonging to the group immunoglobulins (Ig). Each antibody is made up of two kinds of protein chains designated light and heavy (L and H) chains.
The heavy chains are of 5 types:
(i) Gamma,
(ii) Alpha,
(iii) Mu,
(iv) Delta and
(v) Epsilon.
There are thus five classes of immunoglobulins named according to the type of heavy chain present, that is IgG, IgA, IgM, IgD and IgE; of these IgG is most abundant in the serum.
The structure and properties of the different immunoglobulins are genetically controlled. Basically IgG is made up of two light (L) and two heavy (H) chains linked by disulphide bonds. The L chains have 214 and H chains 440 amino acids. Each of the light and heavy chains consists of a constant (C) half and a variable (V) half (Fig. 21.8).
The ability of an organism to produce an enormous number of antibodies lies in the amino acid sequences of the V regions of the light and heavy chains. Thus there are a large number of immunoglobulin chains in which the V region is different but the C region is the same.
The antigen binds to the antibody in the V regions of the light and heavy chains; the combining site determines the specificity for the antigen. The antibody molecule appears V-shaped in the electron microscope. The two antigen-binding sites containing identical amino acid sequences are located at the ends of the two arms. Thus two antigens of the same type can link to a single antibody molecule.
Two questions have been raised, firstly, what genetic mechanisms are responsible for the immense variability of the V region? Secondly are genes coding for the immunoglobulin chains present in the gamete or are produced during somatic differentiation? Proponents of the germ line theory believe that all the immunoglobulin genes are transmitted through the gametes.
There would thus be many different V genes and a large number of copies of one or a few C genes. According to the somatic differentiation theory the variety of V genes is created during lymphocyte differentiation by somatic mutation or by somatic recombination.
The current views combine both the above theories and envision many V genes containing coding sequences and spacers in the germ cells, and a small number of C genes. The innumerable variants of the V genes arise during somatic recombination in the cells of the immune system called B lymphocytes.
There are two types of light chains in the mouse as well as human beings, one called kappa the other lambda, each with a characteristic amino acid sequence. In mouse the variable regions of both kappa and lambda chains are coded by a large number of V genes which have been identified in the DNA of embryonal cells.
There may be several hundred V genes, each gene consisting of two coding regions separated by a silent spacer. The first coding segment is translated into a leader sequence about 20 amino acids long and is thought to be involved in the movement of the antibody across the cell membrane. It is eventually cut off before the antibody molecule is transported.
The second coding region is specific for about 95 amino acids out of the 108 constituting the V region. The remaining 13 amino acids, of the V region are specified by a J gene situated much downstream, that is toward the 3′ end near the gene for the C region.
There is a long non- coded spacer between the V and J genes. When the light chains are of the lambda type in mouse, there are 4 genes for the C region each having its own J gene. The V and C sequences join at the J region to produce the immunoglobulin gene.
Type # 2. The HLA System:
The genetic mechanisms controlling transplantation antigens play a significant role in the organ transplant technique. The treatment of certain human diseases requires transfer of grafts from a host to a recipient individual of a different genetic make-up (allograft). The existence of transplantation antigens first became known from skin grafting experiments in mice.
Whether a graft would be rejected or accepted by the recipient mouse depended upon the presence of histocompatibility antigens present on the skin and other tissue cells. From the results of genetic experiments it was concluded that the histocompatibility antigens were controlled by several different genes, each gene having multiple alleles.
That the red blood cells in humans contain blood group antigens on their surface. These antigens are important in blood transfusions. The white blood cells also carry several antigens which are important in organ transplantation.
These are called histocompatibility antigens and are found to be controlled by four gene loci A, B, C and D on chromosome 6. The histocompatibility (histo meaning tissue) antigens and their corresponding genes constitute the HLA (human leukocyte antigen) system.
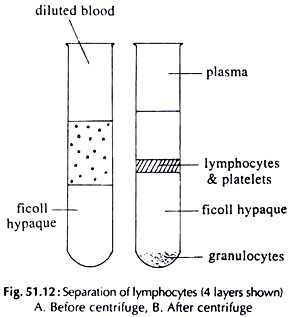
When a graft is transplanted, the lymph nodes of the recipient individual respond to the histocompatibility antigens of the genetically different tissue by producing lymphocytes which are of two types, the T lymphocytes (thymus dependent) and the B lymphocytes (cells equivalent to the bursa in birds).
The T cells are important in graft rejection, and are involved in the cell mediated immune response (CMI). The B cells are involved in the humoral responses (HR) which produce antibodies against viruses, bacteria and such invasions, as well as against graft cells of the host. It is mainly the T cells which respond to the histocompatibility antigens present on the grafted tissue.
The genetics of HLA has been studied by performing breeding experiments in mice. When two mice homozygous for the histocompatibility antigens are crossed, the F1 mice are able to accept grafts from both parents. When F1 mice are inbred, three of the progeny mice accept grafts from either parent, while one mouse shows rejection.
Applying the principles of Mendelian inheritance one can conclude that the parental mice differ at a single gene locus. From similar experiments a number of loci controlling histocompatibility antigens could be determined. Each locus has several alleles. One complex locus H-Z controls the strong transplantation antigens in mouse.
In humans, the strongest transplantation antigens are controlled by four distinct loci A, B, C and D on chromosome 6 (Fig. 21.9). Additional genes related to histocompatibility also lie in the adjacent regions.
Studies on different individuals in the population have revealed that the A gene has more than 12 alleles, and B gene at least 20 alleles controlling more than 32 histocompatibility antigens. As the A and B genes are only one map unit apart, there is very little chance of crossing over between them; they are thus transmitted together in most cases.
Since any allele at A can be associated with any allele at B, the number of possible combinations of the alleles of A and B genes in the population is about 240 (12 x 20). A combination of the alleles of the A and B genes is called the haplotype. Designating the alleles of the A locus as A1, A2, …, A12, and at B as B1, B2,…, B20, suppose one chromosome 6 of a particular individual is carrying the alleles A5 and B9.
The haplotype in this case would be written as 5 9 (A allele is written to the left and B allele to the right). As there are two number 6 chromosomes in a cell, the HLA genotype of a person consists of two haplotypes.
The presence of a particular allele in the individual is determined serologically from the existence of a specific antigen on the leukocyte surface by the technique of leukocyte typing, also called HLA typing. Thus individuals may be homozygous or heterozygous for any pair of alleles.
Due to the highly polymorphic and complex nature of the HLA locus, it is very unlikely that any two persons picked at random should have the same set of leukocyte antigens. These genetic differences lead to rejection of allografts in organ transplantation. Due to this reason the host and recipient HLA genotypes have to be closely matched.
Some Other Loci Linked to HLA:
The gene which is supposed to control the quantity and quality of the immune responses (IR gene) is said to be closely linked to the HLA genes. Some of the immunological disorders are also associated with HLA, such as psoriasis with alleles B8 and B15 of HLA; ankylosing spondylitis with B13 and B7; diabetes mellitus with an allele of the D gene; and multiple sclerosis with alleles of the A, B and D genes.
Type # 3. The Rh Factor:
In 1940, Wiener and Landsteiner discovered that an antigenic factor Rh, which is found on the surface of red blood cells of the Indian brown monkey (Macacus rhesus), is also present in man. They injected the blood of rhesus monkey into rabbits and guinea pigs. Antibodies produced in the blood serum of these animals were found to agglutinate the red cells of the rhesus monkey.
When Landsteiner and Wiener added the same antiserum to human blood, they found to their surprise that the red cells of about 85% of the persons tested were also agglutinated. It was thus revealed that human blood contained the same Rh antigen that was found in the rhesus monkey.
In the same year, Wiener and Peters showed a similarity between the specificity of the animal antibody and an antibody found in the serum of some patients who had shown transfusion reactions. The animal and the human antibodies could both react with the same red cells. The name Rh (after rhesus) was given to the antigen and anti-Rh to the antibody.
Later studies on family pedigrees showed that Rh antigens in humans are controlled by an autosomal dominant gene D. Persons having one or both dominant alleles (DD or Dd) carry Rh or D antigens on their red cells and are said to be Rh positive (Rh+). Persons having two recessive alleles (dd) of the gene lack Rh antigen and are said to be Rh negative (Rh–). There are more than 30,000 Rh or D sites on the surface of each red cell.
As in the case of the ABO blood groups, Rh is also important in blood transfusions. If the blood of an Rh positive person is transfused into an Rh negative person, it will elicit the formation of anti-Rh antibodies in the Rh– recipient. These antibodies will agglutinate the red blood cells of the transfused blood as they carry the Rh antigen on their surface.
The first transfusion of Rh+ blood into an Rh– individual is without severe reaction. But in a subsequent transfusion with Rh+ blood, the sensitized individual will produce increased amounts of antibodies against the Rh antigen in the transfused blood, resulting in severe reaction or even death. It should be noted however, that there are no natural anti-Rh antibodies in the blood of an Rh+ or Rh– individual. Therefore, an Rh– person can donate blood to an Rh+ individual without bad consequences.
Immediately after the discovery of Rh factor, an association was traced between Rh and haemolytic diseases of the newborn (erythroblastosis fetalis) by Levine (1942). These are conditions where newborn infants suffer from anaemia, jaundice, enlarged spleen or liver, in severe cases stillbirth or death soon after birth. This is due to Rh incompatibility between the mother and fetus.
When the mother is Rh negative and carrying two recessive alleles dd of the Rh gene D, and the father is Rh positive, either homozygous DD or heterozygous Dd, then according to Mendelian inheritance the genotype of the foetus could be any one of the following:
If the foetus is dd (Rh–) the pregnancy is normal. Only the Rh+ foetus with Dd genotype creates problems at birth. The gene for Rh (D gene) is transmitted from the father to the foetus (when mother is Rh–).
If the father is homozygous for the D gene (DD), then all the conceptions will produce Rh positive foetuses; if the father is heterozygous (Dd), then there is 50% chance at each conception that the foetus would be Rh+. In addition to the D antigen which distinguishes Rh positive and Rh negative persons, there are other antigens in the Rh system, the main ones being C, E, c and e.
As explained in the case of blood transfusions from Rh+ to Rh– persons, the first pregnancy with an Rh+ foetus may develop low levels of antibody in the mother and remain free of complications. It is also possible for subsequent pregnancies with Rh+ foetus to be normal. This is so because the circulatory systems of the foetus and mother are separate, eliminating any chance for the foetal Rh+ antigen to reach the mother’s blood.
However, problems do arise in second or later pregnancies due to some defect or breakage in the capillaries of the placenta which allows foetal blood to leak into the maternal circulation. This usually happens about the time of birth. In such cases the Rh+ blood of the foetus produces antibodies in the mother’s blood, which may pass back across the placenta into the foetus.
The antibodies react with foetal red cells and cause haemolysis. The reaction may be mild in the first pregnancy with low levels of antibody in the mother’s blood. In subsequent pregnancies in the sensitized woman, another exposure to the Rh+ antigen triggers an immediate response producing high levels of antibody in the blood (Fig. 21.10).
It is possible to treat the woman for prevention of Rh-caused disease in future births. Within 72 hours of the birth of every Rh+ infant, the Rh– mother is given an intramuscular dose of the anti-Rh antibody (Anti-D gamma-globulin), commercially available as RhoGAM.
This antibody destroys the foetal red cells that have entered the mother’s circulation so that they (foetal cells) cannot stimulate the production of anti-D antibodies in the mother. The process is called passive immunisation.
The Genetic Mechanism of Rh:
Rh factor actually comprises a complex group of related antigens known as the Rh system. The genetic mechanisms controlling the Rh system remain confusing. Two genetic models have been proposed, one by Fisher and Race, the other by Wiener. In the Fisher-Race Model, inheritance of Rh is controlled by 3 closely linked genes, designated C, D and E which are present on an autosomal chromosome.
There are two alleles of each gene: C and c, D and d, E and e. An individual could be homozygous or heterozygous for any of the 3 genes. It should be noted that the D gene produces the D antigen, but the allele d does not produce any antigen (silent gene or amorph). All the other alleles C, c, E and e produce their respective antigens.
In the Fisher-Race system, the gene as well as the antigen it produces on the red cell are given the same symbol. If one chromosome of an individual carried the alleles DCe, and the homologous chromosome had DcE at identical loci, the antigens present on the person’s RBCs would be D, C, c, E and e. Each of the antigens can be detected by testing the RBCs with antisera specific for the various antigens.
The Wiener Model:
A somewhat different model has been proposed by Wiener. According to Wiener there is a single gene with multiple alleles (8 major alleles) controlling Rh. The 8 alleles are R°, R1,R2,Rz, r, r1, r” ry. Each gene produces an antigen on the red cell called an agglutinogen. Each agglutinogen can be recognised by reaction with specific antibodies.
Both the models of Fisher-Race and Wiener seem to arrive at the same conclusion. The 3 genes of Fisher-Race can produce 8 different combinations: CDE, CDe, CdE, cDE, cdE, Cde, cDe, cde. The combinations of the alleles of the 3 genes in a way correspond to the 8 alleles of Wiener. Most geneticists use the Fisher-Race system as it is more convenient.