In this article we will discuss about complementary interactions between insulin and glucagon.
Role of Insulin:
Insulin influences carbohydrate metabolism mainly in the liver and muscles. The binding of insulin with the receptor protein may reduce intracellular cAMP in the target cells either by depressing the membrane bond adenylate cyclase or by stimulating the membrane associated phosphodiesterase that destroys cAMP.
The fall in cAMP may depress specific protein kinases and thereby alter ribosomal translation of protein and activates enzymes like phosphorylase and glycogen synthetase.
Physiological actions of insulin exerts following functions regarding carbohydrate metabolism:
1. Glycogenesis:
Insulin stimulates glycogenesis from glucose, in both skeletal muscles and the liver.
This process is initiated by:
(a) Activating protein phosphatase which dephosphorylates and thereby activates glycogen synthetase,
(b) Inducing glycogen synthetase and glucokinase and
(c) By enhancing hexokinase II activity in muscles.
2. Glycogenolysis:
Insulin inhibits breakdown of glycogen to glucose and depresses the release of glucose from the liver into the blood.
This mechanism:
(a) Activates protein phosphatase-l which dephosphorylates and inactivates glycogen phosphorylase.
(b) Represses glucose-6-phosphatase, the final enzyme of the pathway.
3. Gluconeogenesis:
By inhibiting gluconeogen the conversion of amino acids into glucose in the liver hepatic glucose output is reduced. Insulin accomplishes this in two ways—by decreasing the amount of amino acids in the blood that are available to the vit. for gluconeogenesis and by imbibing hepatic enzymes required for converting amino acids into glucose.
Inhibition of gluconeogenesis takes place because it:
(a) Activates protein phosphatase which, dephosphorylates and inactivates fructose 2, 6-bi-phosphatase leading to an increased intracellular concentration of fructose 2, 6-bi-phosphate that allosterically inhibits fructose 1, 6- bi-phosphatase of gluconeogenesis.
(b) Represses pyruvate carboxylase, PEP carboxykinase, fructose 1, 6- bi-phosphatase and glucose-6-phosphatase, all these enzymes lower the transcription rates of their respective genes.
4. Glycolysis:
Insulin enhances glycolysis in muscle, liver, adipocytes etc. because it:
(a) Induces phosphofructokinase-1 and pyruvate kinase of that pathway by enhancing the transcriptions of genes,
(b) Activates a phosphoprotein phosphatase which dephosphorylates and thereby activates pyruvate kinase and
(c) Enhances muscle hexokinase II activity.
5. Glucose transport:
Insulin enhances the rate of glucose transport from extracellular fluid into muscles adipose tissue, mammary glands and other tissues across their plasma membrane. Glucose transport between the blood and cells is accomplished by means of plasma membrane carrier known as glucose transporters (GLUT).
GLUT can be classified into four types according variation of amino acid sequences—GLUT I, II, III and IV. GLUT I transports glucose across the blood brain barrier, GLUT II transfers into the adjacent blood stream the glucose that has entered the kidney and intestinal cells by means of the co transport carriers, GLUT III is the main transporter of glucose into neurons and GLUT IV is the only type of glucose transporter that is responsive to insulin.
Factors Controlling Insulin Secretion:
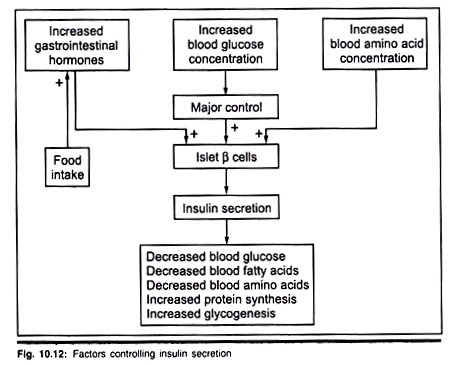
Increased blood glucose concentration, blood amino acids concentration and gastro intestinal hormones are the major controlling factors of insulin secretion. Somatostatin of pancreatic delta cells also controls the secretion of insulin.
Following schematic representation shows the control of insulin secretion (Fig. 10.12).
Role of Glucagon:
Glucagon is an anti-insulin hormone. The most important function is to increase the blood glucose concentration.
This hormone binds to glucagon receptors an the plasma membrane of hepatocytes and adipocytes. Glucagon activates the adenylate cyclase- cAMP system in the membrane to enhance the cytoplasmic concentration of cAMP which acts as the second messenger. cAMP then activates protein kinases which phosphorylate and modulate the activities of specific cellular proteins.
Physiological function of glucagon on carbohydrate metabolism is given below:
1. Glycogenolysis in liver:
Hypoglycemic condition or in starvation, glucagon activates glycogen phosphorylase in the liver to reduce glycogen synthesis. Glucagon has no effect an glycogen phosphorylase of muscle cells.
2. Gluconeogenesis in liver:
Glucagon increases hepatic gluconeogenesis from products of catabolism of proteins (amino acids) by inducing gluconeogenic enzymes like pyruvate carboxylase, fructose 1, 6-di-phosphatase (FD Pase).
3. Inhibition of glycogenesis:
Glucagon suppresses glycogen synthase which in-turn inhibits glycogenesis in liver.
Insulin and glucagon work as a team to maintain blood glucose:
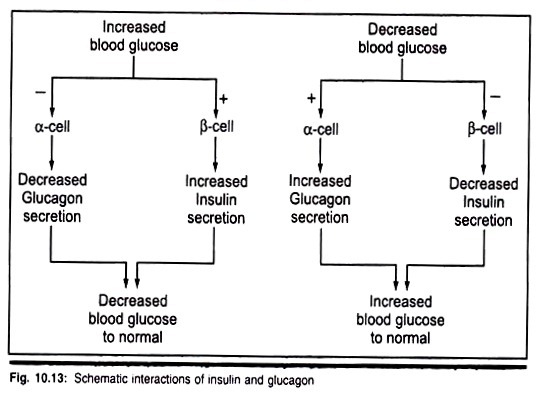
Physiologists believe that the insulin secreting β-cells and the glucagon secreting α-cells as a coupled antagonistic endocrine system whose combined secretory output is a major factor in regulating glucose metabolism. Thus a direct negative feedback relationship between blood glucose concentration and the α-cells rate of secretion, but it is in the opposite direction of the effect of blood glucose on β-cells (Fig. 10.13).
Homeostatic condition of blood glucose level in the blood is maintained insulin and glucagon (Fig. 10.11). Insulin decreases blood sugar level, whereas glucagon increases blood sugar level.
Two physiological conditions are chiefly responsible:
1. During well fed stage:
Dietary carbohydrates stimulate insulin which in-turn stimulates synthesis of glycogen from glucose or glycogenesis. Thus blood glucose is lowered down by activating glycogen synthase.
2. During starvation:
This situation (hypoglycemia) stimulates glucagon secretion and activating hepatic phosphorylase for glycogenolysis. The product glucose is then quickly diffused in the blood to raise sugar level.