In this article we will discuss about:- 1. Introduction to Staphylococcus Aureus 2. The Organism of Staphylococcus Aureus and its Characteristics 3. Pathogenesis and Clinical Features 4. Isolation and Identification 5. Association with Foods.
Contents:
- Introduction to Staphylococcus Aureus
- The Organism of Staphylococcus Aureus and its Characteristics
- Pathogenesis and Clinical Features of Staphylococcus Aureus
- Isolation and Identification of Staphylococcus Aureus
- Staphylococcus Aureus Association with Foods
1. Introduction to Staphylococcus Aureus:
The staphylococci were first described by the Scottish surgeon, Sir Alexander Ogston as the cause of a number of pyogenic (pus forming) infections in humans. In 1882, he gave them the name staphylococcus (Greek: staphyle, bunch of grapes; coccus, a grain or berry), after their appearance under the microscope.
The first description of food poisoning caused by staphylococci is thought to be that of Vaughan and Sternberg who investigated a large outbreak of illness in Michigan believed to have been caused by cheese contaminated with staphylococci.
Clear association of the organisms with foodborne illness had to wait until Barber (1914) demonstrated that staphylococci were able to cause poisoning by consuming milk from a cow with staphylococcal mastitis. In 1930, Dack showed that staphylococcal food poisoning was caused by a filterable enterotoxin.
There are currently 27 species and 7 subspecies of the genus Staphylococcus; enterotoxin production is principally associated with the species Staphylococcus Aureus, although it has also been reported in others including Staph, intermedius and Staph, hyicus.
As a relatively mild, short-lived type of illness, staphylococcal food poisoning is perhaps more likely to be under-reported than others. Most reported cases are associated with outbreaks and only a few sporadic cases are detected.
In the United States between 1983 and 1987, staphylococci accounted for 7.8% (47) of the 600 bacterial food poisoning outbreaks that were recorded. Equivalent figures for England and Wales over the same period were 1.9% (54) out of a total of 2815 outbreaks. Outbreaks of staphylococcal food poisoning in the UK peaked during the 1950s at 150 outbreaks per year but have since declined to an annual level of 10-20 outbreaks.
2. The Organism of Staphylococcus Aureus and its Characteristics:
Staphylococcus aureus is a Gram-positive coccus forming spherical to ovoid cells about 1 µm in diameter. Cell division occurs in more than one plane so that cells form irregular clumps resembling bunches of grapes (Figure 7.6).
Staphylococci are catalase-positive, oxidase-negative, facultative anaerobes. Their ability to ferment glucose can be used to distinguish them from the strictly respiratory genus Micrococcus, although there are species in both genera where this distinction is not clear cut due to low acid production by some staphylococci and production of small amounts of acid under anaerobic conditions by some micrococci.
Enterotoxin production is adversely affected by anaerobic conditions far more than growth.
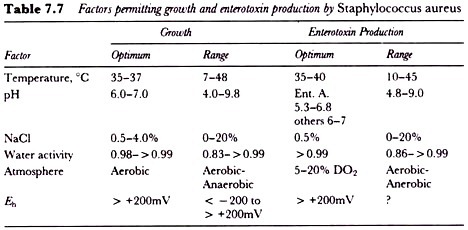
Staphylococcus aureus is a typical mesophile with a growth temperature range between 7 and 48 °C and an optimum at 37 °C under otherwise optimal conditions. The range of temperature over which enterotoxin is produced is narrower by a few degrees and has an optimum at 35-40 °C (Table 7.7).
The organism has unexceptional heat resistance with a D62 of 20-65 s and a D72 of 4.1 s when measured in milk using log-phase cultures. Heat resistance has been shown to vary considerably though, and D values were found to increase three-fold when stationary-phase cultures were tested.
Growth occurs optimally at pH values of 6-7, with minimum and maximum limits of 4.0 and 9.8-10.0 respectively. The pH range over which enterotoxin production occurs is narrower with little toxin production below pH 6.0 but, as with growth, precise values will vary with the exact nature of the medium.
A characteristic of Staphylococcus Aureus which is a particularly important consideration in some foods is its tolerance of salt and reduced aw. It grows readily in media containing 5-7% NaCl and some strains are capable of growth in up to 20% NaCl.
It will grow down to an aw of 0.83 where it has a generation time of 300 min. Once again the range over which enterotoxin production occurs is more limited with a minimum aw recorded of 0.86.
The principal habitat of the staphylococci is the skin, skin glands and the mucous membranes of warm blooded animals. Several species are associated with particular hosts, for example Staph, hyicus with pigs, and Staph, gallinarum with chickens.
Staphylococcus Aureus is more widespread but occurs most frequently on the skin of higher primates. In humans, it is particularly associated with the nasal tract where it is found in 20- 50% of healthy individuals. It can be isolated from faeces and sporadically from a wide range of other environmental sites such as soil, marine and fresh water, plant surfaces, dust and air.
Though normally a harmless parasite of human body surfaces where it plays a useful role metabolizing skin products and possibly preventing skin colonization by pathogens, Staphylococcus Aureus can cause minor skin abscesses such as boils and, more seriously, as an opportunistic pathogen when the skin barrier is breached or host resistance is low.
3. Pathogenesis and Clinical Features of Staphylococcus Aureus:
Food poisoning by Staphylococcus Aureus is characterized by a short incubation period, typically 2-4 h. Nausea, vomiting, stomach cramps, retching and prostration are the predominant symptoms, although diarrhoea is also often reported, and recovery is normally complete within 1-2 days. In severe cases dehydration, marked pallor and collapse may require treatment by intravenous infusion.
The short incubation period is characteristic of an intoxication where illness is the result of ingestion of a pre-formed toxin in the food. Staphylococcus Aureus produces seven protein exotoxins designated A,B,C1,C2,C3,D, and E, some characteristics of which are presented in Table 7.8. Toxin types A and D, either singly or in combination, are most frequently implicated in outbreaks of food poisoning.
In the UK, type A is responsible for 52% of outbreaks, type D for 6%, types A and D combined for 19%, and types C and D combined for 9%. Susceptibility varies between individuals but it has been estimated that in outbreaks less than 1 pg of pure toxin has been required to elicit symptoms. The toxins are small (Mr 27.5-30 kDa) single-chain polypeptides each containing a single disulfide loop near the molecule’s centre.
As a result of their compact structure they are resistant to gut proteases and heat stable, being inactivated only by prolonged boiling. Such procedures would of course eliminate viable Staphylococcus Aureus from a food so it is possible for someone to become ill from eating a food which contains no viable Staphylococcus Aureus.
Though frequently described as enterotoxins the Staphylococcus Aureus toxins are strictly neurotoxins. They elicit the emetic response by acting on receptors in the gut, which stimulate the vomiting centre in the brain via the vagus and sympathetic nerves.
If these nerves are severed then vomiting does not occur. It is not known how the toxin induces diarrhoea but it has been shown not to stimulate adenylate cyclase activity.
4. Isolation and Identification of Staphylococcus Aureus:
The most successful and widely used selective plating medium for Staphylococcus Aureus is the one devised by Baird-Parker in the early 1960s. It combines the virtues of a high degree of selectivity, a characteristic diagnostic reaction, and the ability to recover stressed cells. Lithium chloride and tellurite act as selective agents while egg yolk and pyruvate assist in the recovery of damaged cells.
Reduction of the tellurite by Staphylococcus Aureus gives characteristic shiny, jet-black colonies which are surrounded by a zone of clearing resulting from hydrolysis of the egg-yolk protein lipovitellenin. Colonies also often have an inner white margin caused by precipitation of fatty acid.
Colonial appearance on Baird-Parker (B-P) agar gives presumptive identification of Staphylococcus Aureus which is often confirmed by tests for the production of coagulase and thermo-stable nuclease. Coagulase is an extracellular substance which coagulates human or animal blood plasma in the absence of calcium. It is not specific to Staphylococcus Aureus but is also produced by Staph. intermedius and Staph. hyicus.
Staph. intermedius is unable to reduce tellurite and therefore produces white colonies on B-P agar, but Staph. hyicus, which is found on the skin of pigs and poultry, requires a series of further biochemical tests to distinguish it reliably from Staphylococcus Aureus.
The presence of coagulase can be demonstrated using EDTA-treated rabbit plasma in the tube coagulase test. More rapid test kits are available, based on the detection of bound coagulase (also known as clumping factor) and/or protein A, which reacts with the Fc part of IgG molecules.
Detection is by agglutination of erythrocytes or latex particles coated with fibrinogen or plasma and colonies from selective media can be tested directly, without any intermediate sub-culturing. Coagulase production can also be detected directly in an egg yolk-free modification of B-P agar containing pig or rabbit plasma.
Detection of thermo-stable nuclease uses toluidine blue / DNA agar either with a boiled culture supernatant or as an overlay on heat-treated colonies on B-P agar.
Four biotypes of Staphylococcus Aureus are recognized but the use of bio typing is limited since nearly all of the strains isolated from human sources belong to biotype A. Phage typing schemes are used with Staph. aureus; most food poisoning strains belonging to serogroup III.
Since the enterotoxins will survive heat processes that eliminate the producing organism, toxin detection in a food is a more reliable indication of hazard than viable counting procedures. A number of immunoassay techniques for staphylococcal enterotoxins are available.
Early immunoprecipitation techniques such as the micro-slide gel diffusion test are less sensitive and require lengthy extraction and concentration procedures to isolate sufficient enterotoxin for detection. ELISA techniques which will detect 0.1-1.0 ng toxin g-1 food and reverse passive latex agglutination tests with a sensitivity of 0.5 ng ml-1 are now available and more widely used.
5. Staphylococcus Aureus Association with Foods:
The presence of small numbers of Staphylococcus Aureus on foods is not uncommon. It will occur naturally in poultry and other raw meats as a frequent component of the skin microflora. Similarly, it can be isolated from raw milk where levels may sometimes be elevated as a result of Staphylococcus Aureus mastitis in the producing herd.
As a poor competitor, it normally poses no problem in these situations since it does not grow and is eliminated by cooking or pasteurization. There have however been outbreaks caused by milk products such as dried milk and chocolate milk where growth and enterotoxin production occurred in the raw milk and the enterotoxin, but not the organism, survived subsequent pasteurization.
Though not in itself a health threat, the presence of Staphylococcus Aureus on raw meats does pose the risk of cross-contamination of processed food.
Contamination by food handlers is also probably a frequent occurrence in view of the high rate of human carriage. Colonization of the nose and throat with the organism will automatically imply its presence on the skin and food may also be contaminated from infected skin lesions or by coughing and sneezing.
Since large numbers, typically > 106 g-1, are required for the production of enough toxin to cause illness, contamination is necessary but is not alone sufficient for an outbreak to occur. In particular, temperature and time conditions must also be provided that allow the organism to grow.
Studies in the United States and the UK have found that poultry products and cold, cooked meats are the most common vehicles. Salted meats such as ham and corned beef are particularly vulnerable since the Staphylococcus Aureus is unaffected by levels of salt that will inhibit a large proportion of the competitive flora.
Buffet meals where such meats are served are a common scenario for outbreaks as the food is necessarily prepared some time in advance and too often stored at ambient temperature or inadequately chilled.
Canned foods also offer Staphylococcus Aureus a congenial, competitor-free environment and post-process leakage contamination of cans has been an occasional cause of outbreaks. Other outbreaks have been caused by hard cheeses, cold sweets, custards and cream-filled bakery products. In Japan, rice balls that are moulded by hand are the commonest vehicle while in Hungary, it is ice cream.