In this essay we will discuss about the types of blood groups. Also learn about the importance of blood group studies.
Essay # 1. A, B and O Groups:
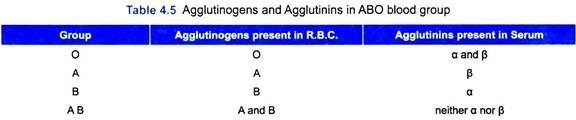
i. The phenomenon of haemoagglutination is due to the interaction between two factors-agglutinogens, present in the corpuscles and agglutinins, present in the plasma (or serum).
ii. There are two primary agglutinogens—A and B; and there are two corresponding agglutinins—α and β. The agglutinogens are inherited as Mendelian dominants, whereas agglutinogens, as recessives.
iii. The corpuscles of a particular subject may contain only A or only B or both A and B or no agglutinogens at all, i.e., O. Similarly, the serum may contain only α or only β or both α and β or no agglutinins, i.e., O.
Agglutinogens start appearing in the sixth week of foetal life. Concentration gradually rises and at birth it reaches one-fourth of the adult level. The adult level is reached at about puberty.
Agglutinogens A and B, are polysaccharides. They are not only found in red cells but in the cells of many other organs, such as salivary glands, pancreas, liver, lungs, testes, etc. They are soluble in water and as such diffuse out into the body fluids.
iv. Thus human beings may be out into four groups according to the nature of the agglutinogens possessed by their corpuscles. These groups are called O, A, B, and AB.
Group A is subdivided into A1 and A2. Group AB is also divisible into A1 B and A2B. Approximately 75-80% of group A belong to the subgroup A1 and 60% of group AB, to the subgroup A1B. The remainder belongs to subgroups A2 and A2B.
Bernstein postulated that there are three allelic genes, A, B, O. Anyone of which can occupy a given position on a chromosome. The O gene is assumed to be recessive and consequently the genotypes AO and BO are expressed as A and B respectively. The finding of subgroups A1 and A2 suggests that there are four alleles, A1, A2, B and O, leading to six phenotypes (Table 4.4). 
The blood group substances are found in many body fluids, saliva and secretions, and Morgan (1948) suggests that this ability to secrete is a Mendelian dominant controlled by a pair of allelic secretor genes— Se.
It is probable, that ABO antigens exist in two groups:
(1) Water-soluble, present in most body fluids under control of Se, and
(2) Alcohol-soluble present in R.B.C but not in secretions.
i. The agglutinin α is again subdivided into α1 and α-proper. α1 reacts with A1, α-proper reacts with both A1 and A2, and β with B; hence α is also known as Anti-A and β as Anti-B respectively. Consequently, ‘A’ cells are not compatible with a-serum and ‘B’ cells are not compatible with β-serum.
ii. From the above it follows that, in the same individual, the agglutinogens in the corpuscles and the agglutinins in the plasma can never be incompatible; otherwise, the red cells would be haemolysed and the subject could not be alive.
The four main ABO group are listed in Table 4.5.
iii. While testing for compatibility the reaction between the donor’s corpuscles and recipient’s plasma, and the donor’s plasma and recipient’s corpuscles should be taken into account.
iv. Taking into consideration all the above facts, the reactions between the red cells and plasma of the four blood groups are summarised in Table 4.6.
v. From the above it is evident that group O can give blood to all but can take only from it own group. Hence, it is called universal donor. Group AB can take blood from all (universal recipient) but can give blood only to its own group. The terms universal donors and universal recipients are no longer applicable after the discovery of Rh factor. Group A and B can give blood to their own groups and also to group AB and can take blood from their own groups and from group O. Other combinations are not compatible (Fig. 4.15).
Frequency of Blood Groups:
A racial difference in the distribution of blood groups has been noted by some workers. Group O has been found to be more common amongst Indian Tribes of America, a section of Australians and Africans, Northwestern Europeans, etc.
White people of America, West Europeans and West Asians have a higher frequency of group A whereas group B is more common in central and South-East Asians, Amongst Indians groups B is highest in North-East (25-30%) and lesser in south (20%). It should be noted that this statistical study is far from being complete.
Group H:
Nearly all human red cells have blood group substance H. In some of them, serum has been found to contain anti-H. Among the ABO groups, group O has the most H material and A1B, the least
Essay # 2. Rh Factor:
Another important agglutinogen has been demonstrated (1940) in human red corpuscles also by Landsteiner and Wiener. It is the agglutinogen of the Rhesus monkey and is present in 85% of White people. Although information is limited, yet it is found that amongst Indians and Ceylonese, the proportion is even larger, about 95% or more. There is no corresponding agglutinin in the human plasma.
Recent studies indicate the Rh factor is not a single entity. There are six Rh agglutinogens—C, c; D, d; E, e. Of these, D and d are the commonest. These two will provide three subgroups—D, Dd and d. D is Mendelian dominant, while d is recessive. Hence, groups D and Dd (collectively called D group) will be Rh positive (Rh+ve) and d will be Rh negative (Rh-ve). Practically all Rh positive people belong to D group and rh negative people to group d.
Clinical Importance:
i. If Rh+ve blood be transfused to a Rh-ve patient, an Anti-Rh factor will develop in the patient’s blood in about 12 days. If a second transfusion of same blood be given to such a patient after this period, haemoagglutination of the donor’s corpuscles will take place. In other words, blood which was compatible before has become incompatible now. So that before transfusion the test for Rh factor should be carefully done.
ii. During pregnancy the foetus may be Rh+ve whereas the mother Rh-ve. The Rh agglutinogen (slightly present also in the plasma) from the foetus passes into the maternal blood and stimulates the formation of Anti-Rh factor. This antibody enters the foetal blood and destroys the red cells of the foetus. The foetus may die (causing miscarriage) or if born alive, suffers from severe anaemia (Erythroblastosis foetalis).
iii. Such a mother becomes sensitised to Rh factor. In future if she gets a transfusion of otherwise compatible blood but containing Rh factor, agglutination will take place.
iv. For the same reason, a Rh negative woman, before menopause should not be give transfusion of Rh positive blood. Because, in cases she becomes pregnant with Rh positive foetus, the problem as described under will become all the more acute.*
Rh Factors Details:
i. Rh Agglutinogens:
There are six or three pairs of Rh agglutinogens—C, c; D, d; and E, e. C, D and E are Mendelian dominants, while c, d and e are recessive.
ii. Human Red Cells:
Human Red cells will always carry three agglutinogens—one from each pair, but they will never carry both the members of any pair. Thus CDE, CDe, cDE are possible but CcD and CDd are not.
iii. Rh group (Genotypes):
It follows therefore that there will be eight possible combinations, any one of which may be carried by both the parents. Hence mathematically, there will be sixty-four possible combinations (genotypes). Of these twenty-eight being identical, thirty-six sub-groups are biologically available. Of these again, only five are commonly found viz., CDe/ CDe, CDe/ cDe,/cde, and cde/ cde. Others are rare.
iv. Rh +ve and Rh-ve:
Groups containing the dominant agglutinogens, i.e., C.D.E. will be Rh+ve. But since, C and E seldom remain without D practically all Rh+ve cases contain D, i.e., belong to group D. The Rh-ve cases will contains the recessive agglutinogens—c, d and e, and due to similar reasons stated above belong to group d. Every man carries some Rh agglutinogen. Majority have D and are Rh+ve. The rest carry d and are rh-ve. All Rh incompatible reactions are due to interactions between group D (donor) and group d (recipient).
v. Rh Antibody:
a. Each of the six agglutinogens has antigenic property, that is, they can stimulate antibody formation. The corresponding antibodies are known as Anti-C, Anti-D, etc. D is strongly antigenic. Others are very feeble.
b. If D cells are repeatedly injected into a Rh-ve subject, Anti-D will develop. This antibody may be of two types early and late. The early Anti-D is formed first and is called complete antibody. It can agglutinate D cells in vitro, when they are suspended either in saline or albumin solution.
Hence, it is also known as saline agglutinin. The late Anti-D is formed later and is called incomplete antibody. It can agglutinate D cells in vitro, when they are suspended in albumin solutions only and not in saline solutions.
Hence, it is also called albumin agglutinin. But in the latter case, though the D cells are not agglutinated, yet they are somewhat modified. Because, these cells once treated in this way, will not be agglutinated by early Anti-D serum, even when they are suspended in albumin solution. Hence, the late Anti-D is also known as the blocking antibody.
c. As mentioned above D is very strongly antigenic. It causes Anti-D formation even by intramuscular injection; so that repeated intramuscular injections of whole blood, as often done in medical practice—without matching the blood groups is not necessarily a safe procedure. Hence, direct cross-matching before each such undertaking is the only surest safeguard.
vi. Racial Distribution:
White people-85% Rh +ve, of which D -35%, Dd-48% and the remaining 2% also contain D along with some other agglutinogen. Indians, Ceylonese—95% Rh+ve. Japanese about 100% Rh+ve. Hence, in the latter, Rh incompatibility reactions are extremely rare.
Haemolytic Disease of the New-Born:
This disease is due to destruction of the Rh+ve R.B.C. in the foetus by an Anti-Rh agglutinin, present in the mother’s serum, which has filtered through the placenta during pregnancy. The incompatibility between the blood of mother and child is caused by the inheritance of the Rh factor.
Incompatibility of the blood might arise only in case marked asterisk (*), in Table 4.7 (as in these two groups the mother is capable of producing an Anti-Rh agglutinin to destroy the Rh+ve R.B.C), present in the foetus.
In this disease, destruction of the normal R.B.C leads to the presence of abnormal nucleated R.B.C in circulation. A few hours after birth there is anaemia, acute jaundice and related symptoms.
Essay # 3. M and N Factors:
Besides the A, B O system, other supplementary agglutinogens have been identified. They are known as M and N factors. This will provide three other independent groups M, N, and MN. These groups are of no importance for blood transfusion but have got medicolegal importance, e.g., paternity test.
There are two blood genes in each person, e.g., M+M, N+N or M+N. If a baby belongs to M group then the parents must have given M+M. If the baby has got N group then the parents must have given N+ N. If the baby belongs to MN group then the parents must have given M+N. In the latter case if the mother’s supplementary group is N then the father must belong to group M. Refer Table 4.8.
This test can only show that the suspected person might or might not be the actual father. In chemical composition, the blood group substances are nitrogenous, neutral, hetero-polysaccharide containing D-galactose, methylpentose fucose, D-glucosamine, D-galactosamine. Present as N-acetyl derivatives and other amino acids such as threonine, serine, protein, etc. The specificity of the blood group substances are dependent on the terminal components which may be non-reducing sugars discussed above.
P System:
Landsteiner and Levine in 1927 demonstrated still another system, P+ and P– by immunisation experiments in rabbits. Subsequently the antigen T1a was found and was shown to be part of the P system. According to some, the P system is a strong system with regularly occurring antibody like Anti-A, Anti-B, etc. But others suggest that the P factor is unimportant in transfusion reactions on haemolytic disease but is important in obstetric case. It is inherited as a Mendelin dominant.
Lutheran, Kell, Duffy, Kidd and other Blood Groups:
Lutheran, Kell, Duffy and Kidd blood groups, spoken of after their names in whose blood they first discovered and were recognized between 1946 and 1951. More have been discovered subsequently, and new blood groups continue to be reported as research in the line progresses.
Importance of Blood Group Studies:
This study is of great value for:
(a) Blood transfusion,
(b) Certain blood diseases,
(c) Paternity test,
(d) In forensic medicine,
(e) Ethnological studies,
(f) Anthropological studies, and
(g) Various experimental purposes.