This article throws light upon the top seven types of immunochemical techniques used in biochemistry for various purposes such as:
(1) Immunoassay:- a biochemical technique that measures the concentration of a substance in a biological liquid;
(2) Radioimmunoassay:- a technique for detecting antigen or antibody;
(3) Enzyme-Linked Immunosorbent Assay:- a technique used for both determining serum antibody concentrations and detecting the presence of antigen or antibody;
(4) Immunoprecipitation :- a technique for detecting a particular antigen in a given cell or tissue type;
(5) Immunoelectrophoresis:- a technique used in clinical laboratories to detect the presence or absence of proteins in the serum;
(6) Immunofluorescence :- a technique used for labelling the antibodies and
(7) Immunohistochemistry:- a technique used for localizing the proteins in cells of a tissue section.
Contents
Technique # 1. Immunoassay:
An immunoassay is a biochemical test that measures the concentration of a substance in a biological liquid, typically serum or urine, using the reaction of an antibody or antibodies to its antigen. The assay takes advantage of the specific binding of an antibody to its antigen.
Monoclonal antibodies are often used as they only usually bind to one site of a particular molecule, and therefore, provide a more specific and accurate test, which is less easily confused by the presence of other molecules. The antibodies selected must have a high affinity for the antigen (if there is antigen available, a very high proportion of it must bind to the antibody).
The presence of both antigen and antibody can be measured. For instance, when detecting infection the presence of antibody against the pathogen is measured. For measuring hormones such as insulin, the insulin acts as the antigen.
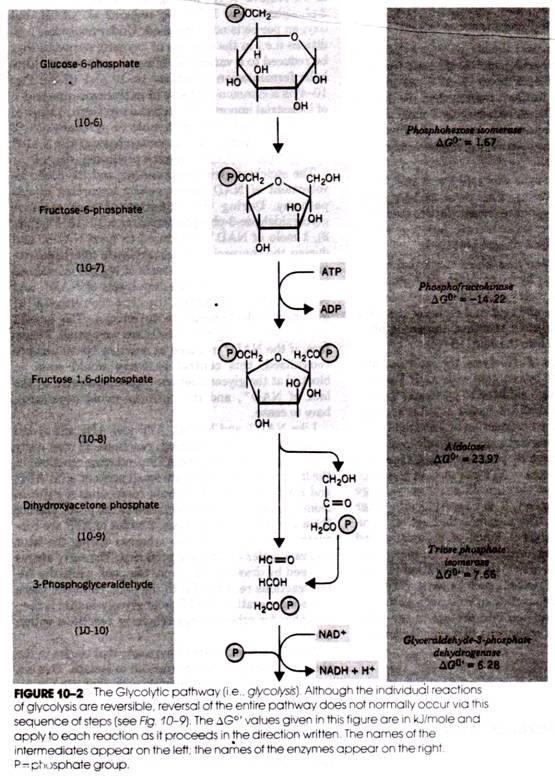
For numerical results, the response of the fluid being measured must be compared to standards of a known concentration. This is usually done through the plotting of a standard curve on a graph, the position of the curve at response of the unknown is then examined, and so the quantity of the unknown is found.
Detecting the quantity of antibody or antigen can be achieved by a variety of methods. One of the most common is to label either the antigen or antibody. The label may consist of an enzyme (see enzyme-linked immunosorbent assay (ELISA)), radioisotopes such as 1-125 Radioimmunoassay (RIA) or fluorescence. Other techniques include agglutination, nephelometry, turbidimetry and Western Blot. Immunoassays have a particularly important role in the diagnosis of HIV through the HIV test.
Types:
Immunoassays can be divided into those that involve labelled reagents and those which involve non-labelled reagents. Those which involve labelled reagents are divided into homogenous and heterogenous (which involved a separation step) immunoassays.
Heterogenous immunoassays can be competitive or non-competitive:
i. In a competitive immunoassay, the antigen in the unknown sample competes with labelled antigen to bind with antibodies. The amount of labelled antigen bound to the antibody site is then measured. In this method, the response will be inversely proportional to the concentration of antigen in the unknown. This is because the greater the response, the less antigen in the unknown was available to compete with the labelled antigen.
ii. In noncompetitive immunoassays, also referred to as the “sandwich assay,” antigen in the unknown is bound to the antibody site, and then labelled antibody is bound to the antigen. The amount of labelled antibody on the site is then measured. Unlike the competitive method, the results of the noncompetitive method will be directly proportional to the concentration of the antigen. This is because labelled antibody will not bind if the antigen is not present in the unknown sample.
Immunoassays can be homogeneous or heterogeneous:
i. A heterogeneous immunoassay will require an extra step to remove unbound antibody or antigen from the site, usually using a solid phase reagent.
ii. Because homogeneous assays do not require this step, they are typically faster and easier to perform.
Technique # 2. Radioimmunoassay (RIA):
One of the most sensitive techniques for detecting antigen or antibody is radioimmunoassay (RIA). The technique was first developed in 1960 by two endocrinologists, S. A. Berson and Rosalyn Yalow, to determine levels of insulin-anti-insulin complexes in diabetics. Although their technique encountered some skepticism, it soon proved its value for measuring hormones, serum proteins, drugs, and vitamins at concentrations of 0.001 micrograms per millilitre or less.
In 1977, some years after Berson’s death, the significance of the technique was acknowledged by the award of a Nobel Prize to Yalow. The principle of RIA involves competitive binding of radiolabelled antigen and un-labelled antigen to a high-affinity antibody. The labelled antigen is mixed with antibody at a concentration that saturates the antigen-binding sites of the antibody.
Then test samples of un-labelled antigen of unknown concentration are added in progressively larger amounts. The antibody does not distinguish labelled antigen from un-labelled antigen, so the two kinds of antigen compete for available binding sites on the antibody. As the concentration of un-labelled antigen increases, more labelled antigen will be displaced from the binding sites.
The decrease in the amount of radiolabelled antigen bound to specific antibody in the presence of the test sample is measured in order to determine the amount of antigen present in the test sample. The antigen is generally labeled with a gamma-emitting isotope such as 1251, but beta-emitting isotopes such as tritium (3H) are also routinely used as labels.
The radiolabelled antigen is part of the assay mixture; the test sample may be a complex mixture, such as serum or other body fluids, that contains the un-labelled antigen. The first step in setting up an RIA is to determine the amount of antibody needed to bind 50%— 70% of a fixed quantity of radioactive antigen (Ag*) in the assay mixture.
This ratio of antibody to Ag* is chosen to ensure that the number of epitopes presented by the labelled antigen always exceeds the total number of antibody binding sites. Consequently, un-labelled antigen added to the sample mixture will compete with radiolabelled antigen for the limited supply of antibody.
Even a small amount of un-labelled antigen added to the assay mixture of labelled antigen and antibody will cause a decrease in the amount of radioactive antigen bound, and this decrease will be proportional to the amount of un-labelled antigen added. To determine the amount of labelled antigen bound, the Ag-Ab complex is precipitated to separate it from free antigen (antigen not bound to Ab), and the radioactivity in the precipitate is measured.
A standard curve can be generated using un-labelled antigen samples of known concentration (in place of the test sample), and from this plot the amount of antigen in the test mixture may be precisely determined. Several methods have been developed for separating the bound antigen from the free antigen in RIA. One method involves precipitating the Ag-Ab complex with a secondary anti-isotype antiserum.
For example, if the Ag- Ab complex contains rabbit IgG antibody, then goat anti-rabbit IgG will bind to the rabbit IgG and precipitate the complex. Another method makes use of the fact that protein A of Staphylococcus aureus has high affinity for IgG. If the Ag-Ab complex contains an IgG antibody, the complex can be precipitated by mixing with formalin-killed S. aureus.
After removal of the complex by either of these methods, the amount of free labelled antigen remaining in the supernatant can be measured in a radiation counter; subtracting this value from the total amount of labelled antigen added yields the amount of labelled antigen bound. Various solid-phase RIAs have been developed that make it easier to separate the Ag-Ab complex from the unbound antigen.
In some cases, the antibody is covalently cross-linked to Sepharose beads. The amount of radiolabelled antigen bound to the beads can be measured after the beads have been centrifuged and washed. Alternatively, the antibody can be immobilized on polystyrene or polyvinylchloride wells and the amount of free labelled antigen in the supernatant can be determined in a radiation counter.
In another approach, the antibody is immobilized on the walls of microtiter wells and the amount of bound antigen is determined. Because the procedure requires only small amount of sample and can be conducted in small 96-well microtiter plates, this procedure is well suited for determining the concentration of a particular antigen in large numbers of samples.
For example, a microtiter RIA has been widely used to screen for the presence of the hepatitis B virus. RIA screening of donor blood has sharply reduced the incidence of hepatitis B infections in recipients of blood transfusions.
Technique # 3. Enzyme-Linked Immunosorbent Assay (ELISA):
Enzyme-linked immunosorbent assay, commonly known as ELISA (or EIA), is similar in principle to RIA but depends on an enzyme rather than a radioactive label. An enzyme conjugated with an antibody reacts with a colourless substrate to generate a coloured reaction product. Such a substrate is called a chromogenic substrate.
A number of enzymes have been employed for ELISA, including alkaline phosphatase, horseradish peroxidase, and β-galactosidase. These assays approach the sensitivity of RIAs and have the advantage of being safer and less costly.
Because the ELISA can be performed to evaluate either the presence of antigen or the presence of antibody in a sample, it is a useful tool both for determining serum antibody concentrations (such as with the HIV test or West Nile Virus) and also for detecting the presence of antigen. It has also found applications in the food industry in detecting potential food allergens such as milk, peanuts, walnuts, almonds, and eggs.
General Method and Instrumentation of ELISA:
The steps of the general, “indirect,” ELISA for determining serum antibody includes:
1. A sample of known antigen is applied to a surface, often the well of a microtiter plate. The antigen is fixed to the surface to render it immobile. Simple adsorption of the protein to the plastic surface is usually sufficient. These samples of known antigen concentrations will constitute a standard curve used to calculate antigen concentrations of unknown samples. Note that the antigen itself may be an antibody.
2. The plate wells or other surfaces are then coated with serum samples of unknown antigen concentration, diluted into the same buffer used for the antigen standards. Since antigen immobilization in this step is due to non-specific adsorption, it is important for the total protein concentration to be similar to that of the antigen standards.
3. A concentrated solution of non-interacting protein, such as Bovine Serum Albumin (BSA) or casein, is added to all plate wells. This step is known as blocking, because the serum proteins block non-specific adsorption of other proteins to the plate.
4. The plate is washed, and a detection antibody specific to the antigen of interest is applied to all plate wells. This antibody will only bind to immobilized antigen on the well surface, not to other serum proteins or the blocking proteins.
5. The plate is washed to remove any unbound detection antibody. After this wash, only the antibody-antigen complexes remain attached to the well.
6. Secondary antibodies, which will bind to any remaining detection antibodies, are added to the wells. These secondary antibodies are conjugated to the substrate-specific enzyme. This step may be skipped if the detection antibody is conjugated to an enzyme.
7. Wash the plate, so that excess unbound enzyme-antibody conjugates are removed.
8. Apply a substrate which is converted by the enzyme to elicit a chromogenic or fluorogenic or electrochemical signal.
9. View/quantify the result using a spectrophotometer, spectrofluorometer, or other optical/electrochemical device.
The enzyme acts as an amplifier; even if only a few enzyme-linked antibodies remain bound, the enzyme molecules will produce many signal molecules. A major disadvantage of the indirect ELISA is that the method of antigen immobilization is non-specific; any proteins in the sample will stick to the microtiter plate well, so small concentrations of analyte in serum must compete with other serum proteins when binding to the well surface. The sandwich ELISA provides a solution to this problem.
ELISA may be run in a qualitative or quantitative format. Qualitative results provide a simple positive or negative result for a sample. The cut-off between positive and negative is determined by the analyst and may be statistical. Two or three times the standard deviation is often used to distinguish positive and negative samples. In quantitative ELISA, the optical density or fluorescent units of the sample is interpolated into a standard curve, which is typically a serial dilution of the target.
Numerous Variants of ELISA:
A number of variations of ELISA have been developed, allowing qualitative detection or quantitative measurement of either antigen or antibody. Each type of ELISA can be used qualitatively to detect the presence of antibody or antigen. Alternatively, a standard curve based on known concentrations of antibody or antigen is prepared, from which the unknown concentration of a sample can be determined.
Indirect ELISA:
Antibody can be detected or quantitatively determined with an indirect ELISA. Serum or some other sample containing primary antibody (Ab1) is added to an antigen-coated microtiter well and allowed to react with the antigen attached to the well. After any free Ab1 is washed away, the presence of antibody bound to the antigen is detected by adding an enzyme-conjugated secondary anti-isotype antibody (Ab2), which binds to the primary antibody.
Any free Ab2 then is washed away, and a substrate for the enzyme is added. The amount of coloured reaction product that forms is measured by specialized spectrophotometric plate readers, which can measure the absorbance of all of the wells of a 96-well plate in seconds. Indirect ELISA is the method of choice to detect the presence of serum antibodies against human immunodeficiency virus (HIV), the causative agent of AIDS.
In this assay, recombinant envelope and core proteins of HIV are adsorbed as solid-phase antigens to microtiter wells. Individuals infected with HIV will produce serum antibodies to epitopes on these viral proteins. Generally, serum antibodies to HIV can be detected by indirect ELISA within 6 weeks of infection.
Sandwich ELISA:
Antigen can be detected or measured by a sandwich ELISA. In this technique, the antibody (rather than the antigen) is immobilized on a microtiter well. A sample containing antigen is added and allowed to react with the immobilized antibody. After the well is washed, a second enzyme-linked antibody specific for a different epitope on the substrate is added, and the coloured reaction product is measured.
Competitive ELISA:
Another variation for measuring amounts of antigen is competitive ELISA. In this technique, antibody is first incubated in solution with a sample containing antigen. The antigen-antibody mixture is then added to an antigen-coated microtiter well. The more antigens present in the sample, the less free antibody will be available to bind to the antigen-coated well.
Addition of an enzyme-conjugated secondary antibody (Ab2) specific for the isotype of the primary antibody can be used to determine the amount of primary antibody bound to the well as in an indirect ELISA. In the competitive assay, however, the higher the concentration of antigen in the original sample, the lower the absorbance.
Chemiluminescence in ELISA:
Measurement of light produced by chemiluminescence during certain chemical reactions provides a convenient and highly sensitive alternative to absorbance measurements in ELISA assays. In versions of the ELISA using chemiluminescence, a luxogenic (light-generating) substrate takes the place of the chromogenic substrate in conventional ELISA reactions. For example, oxidation of the compound luminol by H2O2 and the enzyme horseradish peroxidase (HRP) produces light:
Ab-HRP + Ag → Ab-HRP-Ag luminol + H2O2→ light
The advantage of chemiluminescence assays over chromogenic ones is enhanced sensitivity. In general, the detection limit can be increased at least ten-fold by switching from a chromogenic to a luxogenic substrate, and with the addition of enhancing agents, more than 200-fold. In fact, under ideal conditions, as little as 5 × 10-18 moles (5 attomoles) of target antigen have been detected.
ELISPOT Assay:
A modification of the ELISA assay called the ELISPOT assay allows the quantitative determination of the number of cells in a population that are producing antibodies specific for a given antigen or an antigen for which one has a specific antibody. In this approach, the plates are coated with the antigen (capture antigen) recognized by the antibody of interest or with the antibody (capture antibody) specific for the antigen whose production is being assayed.
A suspension of the cell population under investigation is then added to the coated plates and incubated. The cells settle onto the surface of the plate, and secreted molecules reactive with the capture molecules are bound by the capture molecules in the vicinity of the secreting cells, producing a ring of antigen-antibody complexes around each cell that is producing the molecule of interest.
The plate is then washed and an enzyme-linked antibody specific for the secreted antigen or specific for the species (e.g., goat anti-rabbit) of the secreted antibody is added and allowed to bind. Subsequent development of the assay by addition of a suitable chromogenic or chemiluminescence-producing substrate reveals the position of each antibody- or antigen-producing cell as a point of colour or light.
Technique # 4. Immunoprecipitation:
The immunoprecipitation technique has the advantage of allowing the isolation of the antigen of interest for further analysis. It also provides a sensitive assay for the presence of a particular antigen in a given cell or tissue type. An extract produced by disruption of cells or tissues is mixed with an antibody against the antigen of interest in order to form an antigen-antibody complex that will precipitate.
However, if the antigen concentration is low (often the case in cell and tissue extracts), the assembly of antigen-antibody complexes into precipitates can take hours, even days, and it is difficult to isolate the small amount of immunoprecipitate that forms. Fortunately, there are a number of ways to avoid these limitations.
One is to attach the antibody to a solid support, such as a synthetic bead, which allows the antigen-antibody complex to be collected by centrifugation. Another is to add a secondary antibody specific for the primary antibody to bind the antigen-antibody complexes. If the secondary antibody is attached to a bead, the immune complexes can be collected by centrifugation.
A particularly ingenious version of this procedure involves the coupling of the secondary antibody to magnetic beads. After the secondary antibody binds to the primary antibody, immunoprecipitates are collected by placing a magnet against the side of the tube.
When used in conjunction with biosynthetic radioisotope labelling, immunoprecipitation can also be used to determine whether a particular antigen is actually synthesized by a cell or tissue. Radiolabelling of proteins synthesized by cells of interest can be done by growing the cells in cell-culture medium containing one or more radiolabelled amino acids.
Generally, the amino acids used for this application are those most resistant to metabolic modifications, such as leucine, cysteine, or methionine. After growth in the radioactive medium, the cells are lysed and subjected to a primary antibody specific for the antigen of interest. The Ag Ab complex is collected by immunoprecipitation, washed free of unincorporated radiolabelled amino acid and other impurities, and then analyzed.
The complex can be counted in a scintillation counter to obtain a quantitative determination of the amount of the protein synthesized. Further analysis often involves disruption of the complex, usually by use of SDS and heat, so that the identity of the immunoprecipitated antigen can be confirmed by checking that its molecular weight is that expected for the antigen of interest. This is done by separation of the disrupted complex by SDS-PAGE and subsequent autoradiography to determine the position of the radiolabelled antigen on the gel.
Antibody and soluble antigen interacting in aqueous solution form a lattice that eventually develops into a visible precipitate. Antibodies that aggregate soluble antigens are called precipitins. Although formation of the soluble Ag-Ab complex occurs within minutes, formation of the visible precipitate occurs more slowly and often takes a day or two to reach completion. Formation of an Ag-Ab lattice depends on the valency of both the and body and antigen.
The antibody must be bivalent; a precipitate will not form with monovalent Fab fragments.The antigen must be either bivalent or polyvalent; that is, it must have at least two copies of the same epitope, or have different epitopes that react with different antibodies present in polyclonal antisera. Experiments with myoglobin illustrate the requirement that protein antigens be bivalent or polyvalent for a precipitin reaction to occur.
Myoglobin precipitates well with specific polyclonal antisera but fails to precipitate with a specific monoclonal antibody because it contains multiple, distinct epitopes but only a single copy of each epitope. Myoglobin thus can form a cross linked lattice structure with polyclonal antisera but not with monoclonal antisera.
The principles that underlie precipitation reactions are presented because they are essential for an understanding of commonly used immunological assays. Although various modifications of the precipitation reaction were at one time the major types of assay used in immunology, they have been largely replaced by methods that are faster and, because they are far more sensitive, require only very small quantities of antigen or antibody.
Also, these modern assay methods are not limited to antigen-antibody reactions that produce a precipitate. Table 6.1 presents a comparison of the sensitivity, or minimum amount of antibody detectable, by a number of immunoassays.
Precipitation Reactions in Fluids Yield a Precipitin Curve:
A quantitative precipitation reaction can be performed by placing a constant amount of antibody in a series of tubes and adding increasing amounts of antigen to the tubes. At one time this method was used to measure the amount of antigen or antibody present in a sample of interest. After the precipitate forms, each tube is centrifuged to pellet the precipitate, the supernatant is poured off, and the amount of precipitate is measured.
Plotting the amount of precipitate against increasing antigen concentrations yields a precipitin curve. As Figure 6.8b shows, excess of either antibody or antigen interferes with maximal precipitation, which occurs in the so-called equivalence zone, within which the ratio of antibody to antigen is optimal. As a large multi-molecular lattice is formed at equivalence, the complex increases in size and precipitates out of solution.
As shown in Fig. 6.8, under conditions of antibody excess or antigen excess, extensive lattices do not form and precipitation is inhibited. Although the quantitative precipitation reaction is seldom used experimentally today, the principles of antigen excess, antibody excess, and equivalence apply to many Ag-Ab reactions.
Precipitation Reactions in Gels Yield Visible Precipitin Lines:
Immune precipitates can form not only in solution but also in an agar matrix. When antigen and antibody diffuse toward one another in agar, or when antibody is incorporated into the agar and antigen diffuses into the antibody-containing matrix, a visible line of precipitation will form. As in a precipitation reaction in fluid, visible precipitation occurs in the region of equivalence, whereas no visible precipitate forms in regions of antibody or antigen excess.
Two types of immunodiffusion reactions can be used to determine relative concentrations of antibodies or antigens, to compare antigens, or to determine the relative purity of an antigen preparation. They are radial immunodiffusion (the Mancini method) and double immunodiffusion (the Ouchterlony method);” both are carried out in a semisolid medium such as agar.
In radial immunodiffusion, an antigen sample is placed in a well and allowed to diffuse into agar containing a suitable dilution of an antiserum. As the antigen diffuses into the agar, the region of equivalence is established and a ring of precipitation, a precipitin ring, forms around the well (Fig. 6.9, upper panel). The area of the precipitin ring is proportional to the concentration of antigen.
By comparing the area of the precipitin ring with a standard curve (obtained by measuring the precipitin areas of known concentrations of the antigen), the concentration of the antigen sample can be determined. In the Ouchterlony method, both antigen and antibody diffuse radially from wells toward each other, thereby establishing a concentration gradient. As equivalence is reached, a visible line of precipitation, a precipitin line, forms (Fig. 6.9, lower panel).
Technique # 5. Immunoelectrophoresis:
In Immunoelectrophoresis, the antigen mixture is first electrophoresed to separate its components by charge. Troughs are then cut into the agar gel parallel to the direction of the electric field, and antiserum is added to the troughs. Antibody and antigen then diffuse toward each other and produce lines of precipitation where they meet in appropriate proportions.
Immunoelectrophoresis is used in clinical laboratories to detect the presence or absence of proteins in the serum. A sample of serum is electrophoresed, and the individual serum components are identified with antisera specific for a given protein or immunoglobulin class. This technique is useful in determining whether a patient produces abnormally low amounts of one or more iso types, characteristic of certain immunodeficiency diseases.
It can also show whether a patient overproduces some serum protein, such as albumin, immunoglobulin, or transferrin. The immunoelectrophoretic pattern of serum from patients with multiple myeloma, for example, shows a heavy distorted arc caused by the large amount of myeloma protein, which is monoclonal Ig and therefore uniformly charged.
Because Immunoelectrophoresis is a strictly qualitative technique that only detects relatively high antibody concentrations (greater than several hundred mg/ml), its utility is limited to the detection of quantitative abnormalities only when the departure from normal is striking, as in immunodeficiency states and immunoproliferative disorders.
A related quantitative technique, rocket electrophoresis, does permit measurement of antigen levels. In rocket electrophoresis, a negatively charged antigen is electrophoresed in a gel containing antibody. The precipitate formed between antigen and antibody has the shape of a rocket, the height of which is proportional to the concentration of antigen in the well.
One limitation of rocket electrophoresis is the need for the antigen to be negatively charged for electrophoretic movement within the agar matrix. Some proteins, immunoglobulin’s for example, are not sufficiently charged to be quantitatively analyzed by rocket electrophoresis; nor is it possible to measure the amounts of several antigens in a mixture at the same time. 
Technique # 6. Immunofluorescence:
In 1944, Albert Coons showed that antibodies could be labelled with molecules that have the property of fluorescence. Fluorescent molecules absorb light of one wavelength (excitation) and emit light of another wavelength (emission). If antibody molecules are tagged with a fluorescent dye, or fluorochrome, immune complexes containing these fluorescently labelled antibodies (FA) can be detected by coloured light emission when excited by light of the appropriate wavelength.
Antibody molecules bound to antigens in cells or tissue sections can similarly be visualized. The emitted light can be viewed with a fluorescence microscope, which is equipped with a UV light source. In this technique, known as immunofluorescence, fluorescent compounds such as fluorescein and rhodamine are in common use, but other highly fluorescent substances are also routinely used, such as phycoerythrin, an intensely coloured and highly fluorescent pigment obtained from algae.
These molecules can be conjugated to the Fc region of an antibody molecule without affecting the specificity of the antibody. Each of the fluorochromes below absorbs light at one wavelength and emits light at a longer wavelength. Fluorescein, an organic dye that is the most widely used label for immunofluorescence procedures, absorbs blue light (490 nm) and emits an intense yellow-green fluorescence (517 nm).
Rhodamine, another organic dye, absorbs in the yellow-green range (515 nm) and emits a deep red fluorescence (546 nm). Because it emits fluorescence at a longer wavelength than fluorescein, it can be used in two-colour immunofluorescence assays. An antibody specific to one determinant is labeled with fluorescein, and an antibody recognizing a different antigen is labelled with rhodamine.
The location of the fluorescein-tagged antibody will be visible by its yellow-green colour, easy to distinguish from the red colour emitted where the rhodamine-tagged antibody has bound. By conjugating fluorescein to one antibody and rhodamine to another antibody, one can, for example, visualize simultaneously two different cell-membrane antigens on the same cell.
Phycoerythrin is an efficient absorber of light (~30-fold greater than fluorescein) and a brilliant emitter of red fluorescence, stimulating its wide use as a label for immunofluorescence. Fluorescent-antibody staining of cell membrane molecules or tissue sections can be direct or indirect. In direct staining, the specific antibody (the primary antibody) is directly conjugated with fluorescein; in indirect staining, the primary antibody is un-labelled and is detected with an additional fluorochrome-labelled reagent. A number of reagents have been developed for indirect staining.
The most common is a fluorochrome-labelled secondary antibody raised in one species against antibodies of another species, such as fluorescein-labelled goat anti-mouse immunoglobulin. Indirect immunofluorescence staining has two advantages over direct staining.
First, the primary antibody does not need to be conjugated with a fluorochrome. Because the supply of primary antibody is often a limiting factor, indirect methods avoid the loss of antibody that usually occurs during the conjugation reaction.
Second, indirect methods increase the sensitivity of staining because multiple molecules of the fluorochrome reagent bind to each primary antibody molecule, increasing the amount of light emitted at the location of each primary antibody molecule.
Immunofluorescence has been applied to identify a number of subpopulations of lymphocytes, notably the CD4+ and CD8+ T-cell subpopulations. The technique is also suitable for identifying bacterial species, detecting Ag-Ab complexes in autoimmune disease, detecting complement components in tissues, and localizing hormones and other cellular products stained in situ.
Indeed, a major application of the fluorescent-antibody technique is the localization of antigens in tissue sections or in subcellular compartments. Because it can be used to map the actual location of target antigens, fluorescence microscopy is a powerful tool for relating the molecular architecture of tissues and organs to their overall gross anatomy. 
Technique # 7. Immunohistochemistry:
Immunohistochemistry or IHC refers to the process of localizing proteins in cells of a tissue section exploiting the principle of antibodies binding specifically to antigens in biological tissues. It takes its name from the roots “immuno,” in reference to antibodies used in the procedure, and “histo,” meaning tissue.
Immunohistochemical staining is widely used in the diagnosis and treatment of cancer. Specific molecular markers are characteristic of particular cancer types. IHC is also widely used in basic research to understand the distribution and localization of biomarkers in different parts of a tissue.
Visualizing an antibody-antigen interaction can be accomplished in a number of ways. In the most common instance, an antibody is conjugated to an enzyme, such as peroxidase, that can catalyse a colour-producing reaction.
Alternatively, the antibody can also be tagged to a fluorophore, such as FITC, rhodamine, or Texas Red. The latter method is of great use in confocal laser scanning microscopy, which is highly sensitive and can also be used to visualize interactions between multiple proteins.
Antibody Types:
The antibodies used for specific detection can be polyclonal or monoclonal. Monoclonal antibodies are generally considered to exhibit greater specificity. Polyclonal antibodies are made by injecting animals with peptide antigens and then after a secondary immune response is stimulated, isolating antibodies from whole serum. Thus, polyclonal antibodies are a heterogeneous mix of antibodies that recognize several epitopes.
Antibodies can also be classified as primary or secondary reagents. Primary antibodies are raised against an antigen of interest and are typically unconjugated (un-labelled), while secondary antibodies are raised against primary antibodies. Hence, secondary antibodies recognize immunoglobulin’s of a particular species and are conjugated to either biotin or a reporter enzyme such as alkaline phosphatase or horseradish peroxidase.
Some secondary antibodies are conjugated to fluorescent agents, such as the Alexa-Fluor family, are also frequently used for detection of proteins in IHC procedures. Protein concentration is generally measured by densitometry analysis, where the intensity of staining correlates with the amount of the protein of interest.
Sample Preparation:
In the procedure, depending on the purpose and the thickness of the experimental sample, either thin (about 4-40 µm) slices are taken of the tissue of interest, or if the tissue is not very thick and is penetrable it is used whole. The slicing is usually accomplished through the use of a microtome, and slices are mounted on slides. “Free-floating IHC” uses slices that are not mounted; these slices are normally produced using a vibrating microtome.
Direct and indirect IHC:
There are two strategies used for the immmuno-histochemical detection of antigens in tissue, the direct method and the indirect method. In both cases, the tissue is treated to rupture the membranes, usually by using a kind of detergent, called Triton X-100.
The direct method is a one-step staining method, and involves a labelled antibody (e.g., FITC conjugated antiserum) reacting directly with the antigen in tissue sections. This technique utilizes only one antibody and the procedure is therefore simple and rapid. However, it can suffer problems with sensitivity due to little signal amplification and is in less common use than indirect methods.
The indirect method involves an un-labelled primary antibody (first layer) which reacts with tissue antigen, and a labelled secondary antibody (second layer) which reacts with the primary antibody. (The secondary antibody must be against the IgG of the animal species in which the primary antibody has been raised.) This method is more sensitive due to signal amplification through several secondary antibody reactions with different antigenic sites on the primary antibody. The second layer antibody can be labelled with a fluorescent dye or an enzyme.
In a common procedure, a biotinylated secondary antibody is coupled with streptavidin-horse- radish peroxidase. This is reacted with 3, 3′-Diaminobenzidine (DAB) to produce a brown staining wherever primary and secondary antibodies are attached in a process known as DAB staining. The reaction can be enhanced using nickel, producing a deep purple/gray staining.
The indirect method, apart from its greater sensitivity, also has the advantage that only a relatively small number of standard conjugated (labelled) secondary antibodies need to be generated. For example, a labelled secondary antibody raised against rabbit IgG, which can be purchased “off the shelf,” is useful with any primary antibody raised in rabbit. With the direct method, it would be necessary to make custom labelled antibodies against every antigen of interest.
Diagnostic IHC Markers:
IHC is an excellent detection technique and has the tremendous advantage of being able to show exactly where a given protein is located within the tissue examined. This has made it a widely-used technique in the neurosciences, enabling researchers to examine protein expression within specific brain structures.
Its major disadvantage is that, unlike immuno-blotting techniques where staining is checked against a molecular weight ladder, it is impossible to show in IHC that the staining corresponds with the protein of interest. For this reason, primary antibodies must be well-validated in a Western Blot or similar procedure. The technique is even more widely used in diagnostic surgical pathology for typing tumours (e.g., carcinoma vs. melanoma).
i. Carcinoembryonic antigen (CEA): used for identification of adenocarcinomas. Not specific for site.
ii. CD 15 and CD30 : used for Hodgkin’s disease.
iii. Alpha fetoprotein: for yolk sac tumours and hepatocellular carcinoma.
iv. CD117: for gastrointestinal stromal tumours (GIST).
v. Prostate specific antigen (PSA): for prostate cancer.
vi. Estrogens and progesterone staining for tumour identification.
vii. Identification of B-cell lymphomas using CD20.
Immunotherapy:
Many proteins shown to be highly up-regulated in pathological states by immunohistochemistry are potential targets for therapies utilizing monoclonal antibodies. For example, Her-2/neu (also known as Erb-B2) is highly expressed in a variety of cancer cell types. As such, antibodies against Her-2/ neu have been FDA approved for clinical treatment of cancer under the drug named Herceptin.