Some of the main kinds of Immunity in Animals are as follows:
Animal body is always exposed to various harmful invaders such as bacteria, viruses, fungi, toxins as well as parasites.
Body has an inherent ability to resist all these invaders and toxins. This ability of the organisms to protect themselves against toxins etc. constitutes immunity.
Immunology comprises all the defense mechanisms of the organisms against invaders which tend to damage the tissue and is thus responsible for the protection.
Kinds of Immunity:
Immunity can be subdivided under two heads.
1. Innate immunity:
It includes general defense of body and is also called as natural immunity, native or inherited ones. It is brought about by following means:
(1) First, invaders are eaten up by leucocytes and tissue macrophages by the process so called phagocytosis.
(2) A part of invaders swallowed with food are destroyed by HCl of gastric juice and by digestive enzymes.
(3) Some of the invaders and toxins are destroyed by certain defensive compounds like lysozymes, properdin, basic polypeptides and natural antibodies.
(4) Skin also acts as protective membrane of the body resistant to invading micro-organisms.
Innate immunity makes body resistant to certain animal diseases such as dysentery, cholera, plague, syphilis and measles etc.
Phagocytic system of defense:
Under this category, invading microorganisms are ingested and destroyed by leucocytes of blood and macrophages of connective tissue. The leucocytes reach different parts of body through blood. They can also squeeze through capillary walls by a process – diapedesis.
Neutrophils and monocytes are the most potent phagocytes among which former perform phagocytosis in circulating blood and latter in tissue fluids only. Monocyes are capable of engulfing larger and mere numerous particles than Neutrophils. They form mononuclear phagocytic, reticuloendothelial or tissue macrophage defense system.
As a result of infections or injuries, there occur characteristic sequential changes – inflammation. Damaged tissue releases vasodilators such as histamine, serotonin and bradykinins which increase local blood flow by dilating blood capillaries at the injured sites.
A large quantity of plasma fluids with same proteins leak into affected tissue from capillaries. As a result of these actions, injured site becomes red and swollen resulting in inflammation. Macrophages which are present in the injured tissue start phagocytizing invaders and debris of broken tissue cells.
Thus, they act as first line of defense in innate immunity. Second line of defense includes certain substances release by the inflamed tissue into blood stream. Finally, blood monocytes migrate into tissue and act as third line of defense. During this process, large number of Neutrophils and macrophages are destroyed by invaders. The debris of broken tissue cells along with destroyed Neutrophils forms a creamy paste called pus which is gradually autolyzed and absorbed by tissue.
2. Acquired immunity:
It is also called as adaptive or specific immunity which develops during the life time of an individual and is responsible for special defense against powerful invaders and toxins causing fatal diseases. It may be further actively acquired immunity in which person recovers from infection as a result of antibody production for specific pathogen.
Another passively acquired immunity is temporary one and is accomplished by infusing antibodies or sensitized lymphocytes into body. These foreign antibodies keep the body safe against a possible attack of specific pathogens or antigens.
Acquired immunity falls into two categories:
(i) Humoral immunity
(ii) Cellular immunity
(i) Humoral immunity:
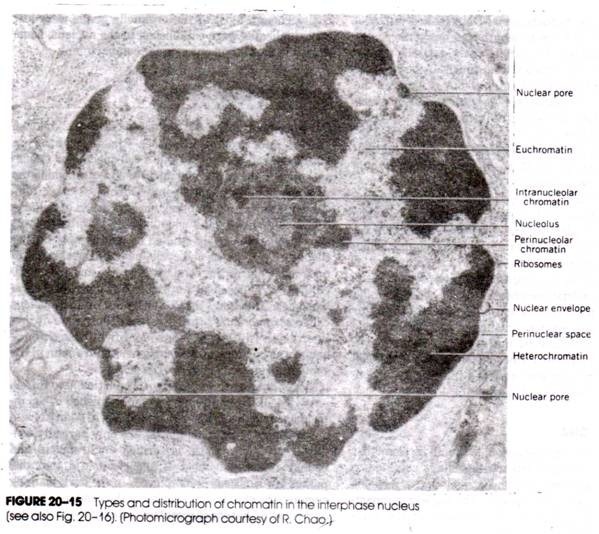
Lymphoid tissue of body which include lymph nodes, spleen, tonsils and bone marrow etc. produce lymphocytes which play active role in acquired immunity responses. Originally, these lymphocytes are derived in late embryo from pluripotent haemopoietic mesodermal stem cells. These stem cells occur initially in yolk sac of embryo and later migrate into embryonic liver, spleen and finally settle in bone marrow. After birth, stem cells proliferate and differentiate into specific “T” and “B” lymphocytes.
In humoral immunity, В lymphocytes reach different parts of the body by blood and are responsible to produce specific antibodies. Generally, В lymphocytes transform into larger cells called plasmocytes or plasma cells in the tissues and these cells produce antibodies.
Remaining daughter lymphocytes are stored as memory cells for future humoral response. Humoral immunity protects the body from fast-occurring diseases such as cholera, cold, tetanus, smallpox etc.
(ii) Cellular immunity:
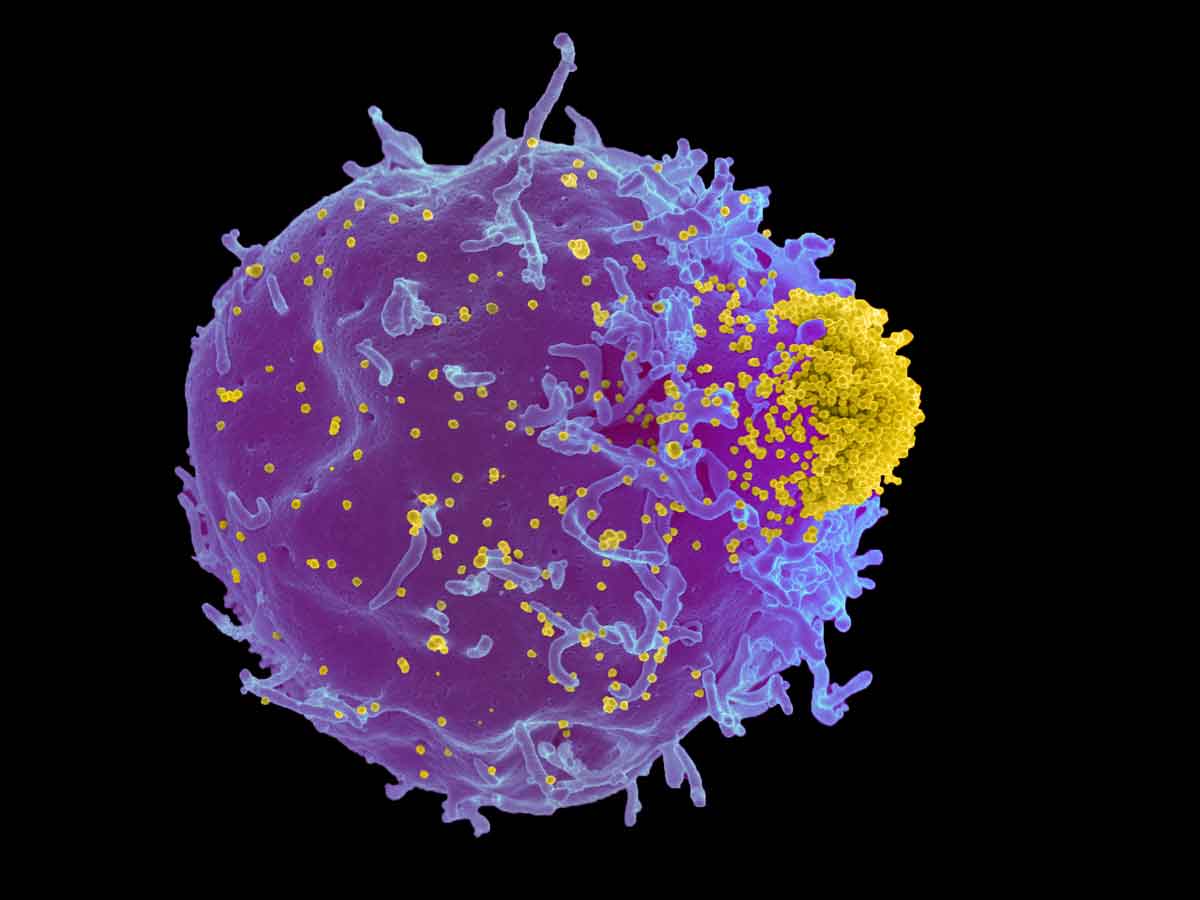
Unlike humoral immunity where body develops circulating antibodies (immunoglobulins) capable of attacking antigens (microorganisms or toxins), cellular immunity refers to production of large number of specifically sensitized lymphocytes (T-lymphocytes) which attack and destroy specific invaders. T-lymphocytes originally derived from stem cells migrate into thymus and become differentiated into various T-lymphocytes. Thymus is a primary lymphoid organ where immature precursor stem cells mature into T cells.
Lymph nodes, spleen and Peyer’s patches represent secondary lymphoid tissue in which T cells are activated by foreign peptide – MHC complex. Histologically, thymus consists of three regions. Outer sub capsular zone is thin and possesses immature T cells precursors along with CD 4, CD 8 receptors.
Afterwards, these T cells precursors enter cortex region of thymus where MHC molecules get expressed. Selected T cells finally enter medulla region of thymus where final differentiation into CD4+ or CD8+ takes place. From medulla, these cells enter blood and reach secondary lymphoid organ where they become activated by a foreign peptide – MHC complex.
Cellular immunity protects body from gradually – progressing diseases like cancer, leprosy and tuberculosis.
T-lymphocytes:
As mentioned above, T cells develop in the thymus and are responsible for cellular immunity. The plasma membrane of a T cell contains receptor proteins which recognize specific antigen. In some cases, T cells may secrete chemical signals in the form of interleukins, lymphokines or interferons (antiviral substance) which stimulate macrophages to destroy the invading microorganisms. T cells may be of following types:
(i) Cytotoxic (killer) T cells
(ii) Helper T cells
(iii) Suppressor T cells
(i) Cytotoxic (killer) T cells:
These kill the cells which are infected with a virus or microorganism. This killing of target cell by cytotoxic T cells is facilitated by a protein called talin that links T cell receptors with cortical actin filaments. Afterwards, cytotoxic T cells secrete pore-forming proteins called perforins. They punch large round holes in the membrane of attacked cell thus helping in the formation of transmembrane channel.
T cell receptors are specific proteins found on the plasma membrane of T cells and meant for recognition of particular antigen. Each receptor consists of two polypeptide chains called a and (3 being linked with disulphide bonds.
Generally, T cells respond to the presence of some peptide fragments present on the surface of infected target cell. These peptide fragments are carried to cell surface by specific proteins so called major histocompatibility complex or MHC molecules.
They are of two types i.e. МНС -I and MHC-II molecules. MHC-I molecules consist of single polymorphic transmembrane polypeptide chain called α-chain with an extracellular protein β2 -microglobulin, MHC-I molecules are found on all nucleated cells and involved in binding peptide fragments from intracellular antigens – virus and presenting the cells to cytotoxic T cells. On the other hand, MHC-II molecules occur on specialized cells like thymocytes, В-cells and are involved in the binding of extracellular peptide fragments and presenting them to helper T cells.
(ii) Helper T cells:
The helper T cells are most numerous consisting of about 75% of T cells. They help in the functions of immune system in many ways. AID virus inactivates or destroys helper T cells thus leaving body totally unprotected against infectious diseases.
The helper T cells are of two types: Th1 cells which activate macrophages and Th2 cells that stimulate В cells to make antibodies and facilitate the action of other T cells. Therefore, the helper T cells control immunity indirectly. They are recognized by MHC -II molecules and usually two signals are required for activation of helper T cells. The chemical signal or interleukin – 1 (1L-I) and another B7 + CD 28 protein activates helper T cells which in turn secrete a variety of lymphokines or cytokines.
The lymphokines are secreted by some helper T cells which act as messenger molecules that recruit other leucocytes to the battle site. They don’t bind antigens and therefore mediate local interactions between white blood cells.
Important lymphokines include interleukins (2, 3, 4, 5, and 6), granulocyte – monocyte colony stimulating factor and interferons. Besides their own proliferation helper T cells (Th1) also activate cytotoxic T cells and Th2 cells help В cells and eosinophils.
(iii) Suppressor T cells:
These cells protect body’s own cells from attack so called immune tolerance. They guard against overproduction of antibodies and over activity of cytotoxic T cells. Therefore, suppressor T cells cause both В cells and other T cells to become less active. Sometimes they along with helper T cells are designated as regulator T cells. Many of the suppressor T cells remain stored in lymph nodes and spleen and become memory cells.