The physiological properties of the cardiac muscle are: 1. Rhythmicity 2. Excitability 3. Contractility 4. Conductivity.
Property # 1. Rhythmicity/Automaticity/Chronotropism:
In the myocardium, automaticity is the ability of the cardiac muscles to depolarize spontaneously, without external electrical stimulation from the nervous system.
i. Primary Pacemaker:
The sinoatrial node (SA node) is a group of cells positioned on the wall of the right atrium, near the entrance of the superior vena cava. These cells are modified cardiac myocytes. They possess some contractile filaments, though they only contract relatively weakly.
Cells in the SA node spontaneously depolarize, resulting in contraction, approximately 100 times per minute. This native rate is constantly modified by the activity of sympathetic and parasympathetic nerve fibers, so that the average resting cardiac rate in adult humans is about 70 beats per minute. Because the sinoatrial node is responsible for the rest of the heart’s electrical activity, it is sometimes called the primary pacemaker.
ii. Secondary Pacemaker:
If the SA node does not function, a group of cells further down the heart will become the heart’s pacemaker, this is known as an ectopic pacemaker. These cells form the atrioventricular node (AV node), which is situated beneath the endocardium at the lower right posterior portion of the interatrial septum near the opening of the coronary sinus above the tricuspid valve.
The cells of the AV node normally discharge at about 40-60 beats per minute, and are called the secondary pacemaker.
iii. Tertiary Pacemaker:
Further down the electrical conducting system of the heart is the bundle of His. The left and right branches of this bundle, and the Purkinje fibers, will also produce a spontaneous action potential at a rate of 30-40 beats per minute, if the SA and AV node both do not function.
The reason the SA node controls the whole heart is that its action potentials are released most often to the heart’s muscle cells; this will produce contraction. The action potential generated by the SA node passes down the cardiac conduction system, and arrives before the other cells have had a chance to generate their own spontaneous action potential. This is the normal conduction of electrical activity within the heart.
Generation of Action Potentials:
There are three main stages in the generation of an action potential in a pacemaker cell.
They are:
a. Pacemaker Potential:
The key to the rhythmic firing of pacemaker cells is that, unlike muscle and neurons, these cells will slowly depolarize by themselves.
The resting potential of a pacemaker cell (-55 mV to -60 mV) is caused by a continuous outflow or “leak” of potassium ions through ion channels in the membrane. This potassium permeability decreases as time goes on, partly causing the slow depolarization. As well as this, there is a slow inward flow of sodium, called the funny current, as well as an inward flow of calcium, through transient Ca2+ channel (T-channel). This all serves to make the cell more positive.
This relatively slow depolarization continues until the threshold potential is reached. Threshold is between -40 mV and -50 mV. When threshold is reached, the cells enter phase of depolarization.
b. Depolarization:
Though much faster than the depolarization caused by the funny current and decrease in potassium permeability above, the upstroke in a pacemaker cell is slow, as compared to that in an axon.
The SA and AV node do not have fast sodium channels like neurons, and the depolarization is mainly caused by a slow influx of calcium ions. (The funny current also increases). The calcium is let into the cell by voltage-sensitive calcium channels (long lasting or L-type channel) that open when the threshold is reached.
c. Repolarization:
The calcium channels are rapidly inactivated, soon after they open. Sodium permeability is also decreased. Potassium permeability is increased, and the efflux of potassium (loss of positive ions) slowly repolarises the cell.
Factors Affecting Myocardial Rhythmicity:
1. Cardiac Innervation:
a. Sympathetic Stimuli:
It releases noradrenaline, which acts on the beta 1 receptors causing rapid opening of Ca channels, accelerating the rate of depolarisation. As a result, the slope of depolarization increases, causing increased rate of SA node firing and increased heart rate.
b. Parasympathetic Stimuli (Vagus):
It releases acetylcholine which acts on the muscarinic receptors, causing opening of K+ channels, increases SA node membrane permeability to K+ results in more K+ efflux and decreased membrane permeability to Ca2+ results in less Ca2+ influx. As a result, the pre- potential slope decreases, causing decreased rate of SA node firing and decreased heart rate.
2. Effect of Ion Concentrations in ECF:
a. K+ Ions:
Decreased K+ increases rhythmicity. Increased K+ decreases rhythmicity (stops heart in diastole).
b. Na+ Ions:
If increased, initiate rhythmicity, but cannot maintain it.
3. Physical Factors:
a. Warming ― Increases rhythmicity
b. Cooling ― Decreases rhythmicity.
c. Exercise ― Increases heart rate as a result of increased sympathetic nerve stimulation and decreased vagal inhibition to SA node.
d. Endurance-trained athletes ― Resting bradycardia due to high vagal activity.
4. Chemical Factors (Drugs):
a. Thyroid hormones and catecholamine ― Increases rhythmicity.
b. Acetylcholine decreases rhythmicity.
c. Hypoxia ― Decreases rhythmicity.
Property # 2. Excitability (Bathmotropism):
Is the ability of cardiac muscle to respond to adequate stimuli by generating an action potential.
Action Potential of Ventricular Muscle:
i. Ventricular muscle has a resting membrane potential of -90 mV.
ii. The transmembranous action potential overshoots to a potential of +20 mV.
iii. Transmembranous action potential of ventricular muscle is characterized by presence of 5 phases. Phase 0 = Rapid depolarization.
iv. Opening of fast Na+ channels increased Na+ influx. Phase 1 = Rapid repolarization/1st rapid repolarization.
v. Closure of Na+ channels, decreased K+ permeability, and CI– influx.
Phase 2 = A plateau.
vi. Opening of slow Ca2+ channels (slow Ca2+ Na+ channels) increased Ca2+ influx, with slow opening of K+ channels.
Phase 3 = Slow repolarization/2nd rapid repolarization.
vii. Closure of slow Ca2+ channels, with increased K+ permeability increased K+ efflux.
Phase 4 = Complete repolarization.
viii. Active Na+ K+ pump 2K+ in/3Na+ out.
Excitability changes during the action potential
Passes through 2 periods:
1. Absolute refractory period (ARP)
2. Relative refractory period (RRP).
Refractory Periods:
1. Absolute Refractory Period (ARP):
i. The excitability of cardiac muscle is completely lost during this period, i.e. does not respond to 2nd stimulus however strong it may be.
ii. The duration is very long that occupies the whole period of systole.
iii. Corresponds to the period of depolarization (phase 0), and the first 2 phases of repolarization.
iv. Heart cannot be tetanized (continuous contraction), as its ARP occupies the whole contraction phase.
2. Relative Refractory Period (RRP):
i. The excitability of cardiac muscle is partially recovered during this period, i.e. stronger stimuli than normal are required to excite the muscle.
ii. Occupies the time of diastole.
iii. Corresponds to the 3rd phase of repolarization.
iv. Can be affected by the heart rate, temperature, vagal stimulation, sympathetic stimulation and drugs.
Extrasystole and Compensatory Pause:
The refractory periods can be demonstrated in the beating heart of frog. If a stimulus is applied during systole, there is no response. If stimulus is applied during diastole, there is a contraction called extrasystole, which is of higher amplitude due to beneficial effect. The extrasystole is followed by a compensatory pause.
This pause occurs because when the next normal impulse from the sinus arrives, the heart is in absolute refractory period of extrasystole. Therefore, it has to wait for the next normal impulse to arrive. The interval between the contractions preceding and following the extrasystole is equal to the length of 2 cardiac cycles.
Postextrasystolic Potentiation:
Ventricular extrasystole increases myocardial contractility so that the contraction following the extrasystole is stronger than the contraction preceding it. This is mainly due to greater availability of Ca++ ions resulting from previous contraction. This is called as postextrasystolic potentiation.
Factors Affecting Myocardial Excitability:
1. Cardiac Innervation:
i. Sympathetic nerve stimulation increases excitability.
ii. Parasympathetic nerve stimulation (vagus) decreases excitability.
2. Effect of Ions Concentration in ECF:
i. Increased Ca2+ and increased Na+ → increases excitability.
ii. Increased K+ → increases excitability.
3. Physical Factors:
i. Rise in temperature increases excitability.
ii. Decrease in temperature decreases excitability.
4. Blood Flow:
Insufficient blood flow to cardiac muscle decreases excitability and myocardial metabolism for three reasons:
a. Lack of O2
b. Excess accumulation of CO2
c. Lack of sufficient food nutrients.
5. Chemical Factors (Drugs):
Digitalis increases excitability.
Relation between the Actions Potential and the Mechanical Response:
i. The mechanical response consists of contraction (systole) and relaxation (diastole).
ii. Cardiac muscle begins to contract a few milliseconds after the action potential begins, and continues to contract until a few milliseconds after the action potential ends.
iii. Duration of contraction ― 0.2 sec in atrial muscle, and 0.3 sec in ventricular muscle.
iv. Diastole begins at the end of the plateau.
2nd rapid repolarization is completed at about the middle of diastole.
Property # 3. Contractility/Inotropism:
It is the ability of the cardiac muscle to convert electrical energy into mechanical work. Myocardial fibers have ‘functional syncytium’ and not ‘anatomical syncytium’, because they present in contact but not in continuity.
i. Strength of myocardial contraction determines the heart pumping power.
ii. Mechanism of contraction depends on the contractile filaments, which contain the protein molecules (actin and myosin).
Excitation-Contraction Coupling in Cardiac Muscle:
Is the mechanism by which action potential causes myofibrils of cardiac muscle to contract. When action potential passes over cardiac muscle membrane, it also spreads to interior of cardiac muscle fiber along membranes of transverse (T) tubules. Extracellular Ca2+ diffuses down gradient into cell through T- tubules. This Ca2+ stimulates opening of Ca2+ channels in sarcoplasmic reticulum (calcium induced calcium release).
Finally, the Ca2+ released from here, binds to troponin and stimulates contraction (same mechanisms as in skeletal muscle). At the end of plateau of cardiac action potential, i.e. during repolarization, Ca2+ in sarcoplasm is rapidly and actively transported and pumped out of the cell via a Na+– Ca2+– exchanger, back into both sarcoplasmic reticulum and T-tubules resulting in cessation of the contraction until new action potential occurs.
Factors affecting Myocardial Contractility:
1. Cardiac Innervation:
i. Sympathetic nerve stimulation increased force of contraction.
ii. Parasympathetic nerve stimulation (vagus) decreased atrial force of contraction with no significant effect on ventricular muscle.
2. Oxygen Supply:
Hypoxia decreases contractility.
3. Calcium and Potassium Ions Concentration in ECF:
i. Increase in Ca2+ increases contractility.
ii. Increase in K+ increases contractility.
4. Physical Factors:
i. Warming increases contractility.
ii. Cooling decreases contractility.
5. Hormonal and Chemical Factors (Drugs):
i. Positive inotropics ― (Adrenaline, noradrenaline, alkalosis, digitalis, Ca2+, caffeine).
ii. Negative inotropics ― [Acetylcholine, acidosis, ether, chloroform, some bacterial toxins (e.g. diphtheria toxins), K+].
Characteristics of Contractility:
a. Cardiac muscle obeys ‘all-or-none law’. A single sub-minimal stimulus does not evoke any response, but minimal or threshold stimuli lead to maximal cardiac contraction, and further increase in stimulus strength does not increase the contraction.
b. Cardiac muscle cannot be stimulated while it is contracted, because its excitability during contraction is zero due to long absolute refractory period, so it cannot be tetanized.
c. Cardiac muscle can perform both isometric and isotonic types of contractions.
d. Starling’s law of the heart “Length-tension relationship”. Within physiological limits, the greater the initial length of the fiber, the stronger will be the force of its contraction; however, overstretching the fiber as in heart failure its power of contractility decreases.
e. Staircase phenomenon/Treppe ― If several adequate stimuli of same strength are applied in quick succession, the first few contractions show a progressive increase in amplitude, after that it becomes standstill. The initial increase is due to increase of temperature, H+ ion and Ca++ ion concentrations resulting from previous contractions. This is referred to as staircase phenomenon.
f. Summation of sub-minimal stimuli. A single sub-minimal stimulus is ineffective. But if two or more such stimuli are applied in quick succession, there is a response. This is due to summation of all the local excitatory states caused by each sub-minimal stimulus.
Property # 4. Conductivity (Dromotropism):
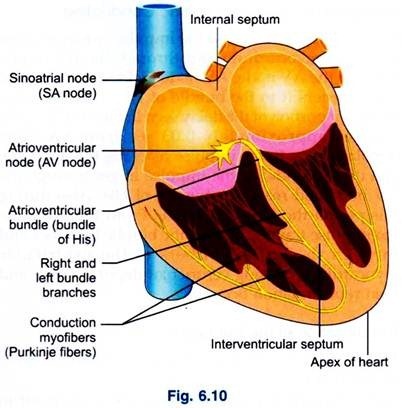
Is the ability of cardiac muscle fibers to conduct the cardiac impulses that are initiated in the SA node (the pacemaker of the heart) (Fig. 6.10).
1. SA Node:
Under normal conditions, electrical activity is spontaneously generated by the SA node, the physiological pacemaker. This electrical impulse is propagated throughout the right atrium, and through Bachmann’s bundle to the left atrium, stimulating the myocardium of both atria to contract. As the electrical activity is spreading throughout the atria, it travels via specialized pathways, known as internodal tracts, from the SA node to the AV node.
2. Internodal Tracts:
They comprise of three namely, anterior bundle of Bachmann, middle-Wenkebach, and posterior bundle of Thorel.
3. AV Node:
The AV node functions as a critical delay in the conduction system. Without this delay, the atria and ventricles would contract at the same time, and blood would not flow effectively from the atria to the ventricles.
4. Bundle of His:
The distal portion of the AV node is known as the bundle of His. The bundle of His splits into two branches in the interventricular septum, the left bundle branch and the right bundle branch. The left bundle branch activates the left ventricle, while the right bundle branch activates the right ventricle. The left bundle branch is short, splitting into the left anterior fascicle and the left posterior fascicle.
5. Purkinje Fibers/Ventricular Myocardium:
The two bundle branches taper out to produce numerous Purkinje fibers, which stimulate individual groups of myocardial cells to contract.
Sequence of Events in Cardiac Conduction:
SA node depolarizes and the impulse spreads across the atrial myocardium and through the internodal fibers to the AV node. AV node picks up the impulse and transfers it to the bundle of His. This produces the major portion of the delay seen in the cardiac cycle.
It takes approximately 0.03 sec from SA node depolarization to the impulse reaching the AV node, and 0.13 seconds for the impulse to get through the AV node and reach the bundle of His. Also during this period the atria repolarize. From the AV node the impulse travels through the bundle branches and through the Purkinje fibers to the ventricular myocardium, causing ventricular depolarization and then repolarization occurs.
The Direction of the Impulse (Fig. 6.11):
1st → Atrial spread from SA node conductive tissue to ventricles
2nd → Ventricular spread from apex of the heart to base, via Purkinje fibers to the endocardial surface of ventricles.
Note:
Left bundle branch starts before right bundle branch, as left ventricular wall is thicker so the impulse needs more enough time to reach. Accordingly both ventricles will contract together.
The Conduction Velocities of the Impulse:
SA node – 0.05 m/sec
AV node – 0.01 m/sec (slowest)
Bundle of His – 1.00 m/sec
Purkinje fibers – 4.00 m/sec (fastest)
Atrial and ventricular muscles – 0.3 to 0.4 m/sec
The slowest conduction velocity in AV node: Because it has few number of intercalated discs.
Importance ― To allow sufficient time for ventricles to be filled with blood before they contract.
The fastest conduction velocity in Purkinje fibers
Importance ― To allow the 2 ventricles to contract at the same time simultaneously.
Factors affecting Myocardial Conductivity:
1. Cardiac Innervation:
i. Sympathetic nerve stimulation ― Increases conductivity.
ii. Parasympathetic nerve stimulation (vagus) ― Decreases conductivity.
2. Effect of Ions Concentration in ECF:
i. Increase in Ca2+ → Increases conductivity.
ii. Increase in K+ → Increases conductivity.
3. Physical Factors:
i. Rise of temperature increases conductivity.
ii. Decreases temperature decreases conductivity.
4. Blood Flow:
Insufficient blood flow to cardiac muscle decreases conductivity and myocardial metabolism for three reasons:
i. Lack of O2
ii. Excess accumulation of CO2
iii. Lack of sufficient food nutrients.
5. Chemical Factors (Drugs):
Digitalis → Increases conductivity.