The following points highlight the ten main varieties of connective tissues of human body. They are: 1. Areolar Tissue 2. Adipose Tissue 3. White Fibrous Tissue 4. Yellow Elastic Tissue 5. Reticular Tissue 6. Blood and Haemopoietic Tissue 7. Cartilage 8. Jelly-Like Connective Tissue 9. Osseous Tissue or Bone 10. Reticulo-Endothelial Tissue.
1. Areolar Tissue:
Distribution:
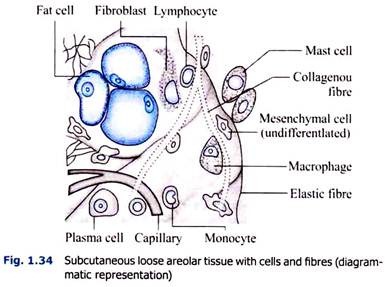
(a) In the subcutaneous (Fig. 1.34), submucous and subserous tissues;
(b) Between muscles, vessels and nerves;
(c) In the interior of organs binding the different parts. Aerolar tissues is composed of fibres and cells.
Fibres are:
(a) White or collagenous.
(b) Yellow elastic fibres.
(c) Reticular fibres (Fig. 1.35).
The bundles of collagenous, elastic and reticular fibres cross and intercross, thus making a network, the places of which are occupied by the clear ground substance and various types of cells (Flow chart 1.3). Following varieties of cells are generally found in the aerolar tissue.
2. Adipose Tissue (Fig. 1.36):
Description: The adipose or loose tissue is characterised by containing free fat inside the fat cells. These cells remain supported by a loose framework of areolar tissue. The cells are generally large, rounded or oval in shape. They may be polyhedral due to pressure of the adjacent fat cells. The big fat droplets occupy almost the whole of the cell.
The cytoplasm and the flattened nucleus are pushed out to one side. For this reason the cell looks like a ‘signet ring. The fat cells may be stained by Sudan III or Scharlach R or osmic acid. In paraffin sections, the fat droplets are dissolved out and the cells look like big white gaps. Blood vessels and lymphatics pass along the loose framework. The cells are said to contain special enzymes which help deposition of neutral fat.
On morphological ground there are:
i. White or yellow (unilocular) adipose tissue which comprises the bulk of body’s fat reserves, and
ii. Brown (multilocular) adipose tissue is much more restricted in its distribution.
Distribution:
They remain distributed in many places and are specially found in the so-called fat depots, via., omentum, subcutaneous tissue, mesentery and perinephric region, subpericardial tissue, etc. yellow bone marrow is very rich in fat. The lactating mammary gland contains a large amount of fat. Adipose tissue is absent in eyelids, penis, scrotum, labia minora, cavity of cranium, lungs except their roots etc.
Functions:
i. Remaining under the surface gives shape to the limbs and body.
ii. Remaining around the viscera keeps them in position and prevents injury.
iii. Plays a good part in the regulation of body temperature.
iv. Represents stored energy (Vide also Depot Fat).
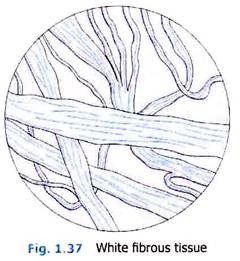
3. White Fibrous Tissue (Fig. 1.37):
It is made up of shining white fibres (formed by the fibroblasis). They are thin and non-branching (regular). The fibres do not run singly but in bundles. The bundles of white fibres are wavy (irregular) and run in different directions. Although the individual fibres do not branch, yet the bundles freely branch and the branches communicate with one another.
The interspaces thus produced are occupied by areolar tissue ‘ and the connective tissue corpuscles. These cells become squeezed by the adjacent bundles of white fibres and in transverse section assume an angular stellate appearance. Such stellate cells are typically found in the transverse section of tendons.
Distribution:
White fibrous tissue is present in tendons, ligaments, aponeurosis, articular capsule, the deep fascia of the body and limbs, the fibrous coverings of the organs and certain other membranes, e.g., the duramater, etc. It is also found in one form the fibro cartilage.
Functions:
It connects the different tissues and the different parts of the body to afford mechanical protection against stretch and pressure, and in this way to impart great strength as well as a considerable amount of flexibility. Chemically, white fibrous tissue is made up of a protein known as collagen (Fig. 1.38), digestible with pepsin. From this, gelatin is easily obtained by boiling with a little hydrochloric acid. Electron microscopic studies revealed the fundamental molecule of collagen to be tropocollagen, about 3000 Å in length and 15 Å in width.
4. Yellow Elastic Tissue (Fig. 1.39):
This is another variety of fibrous tissue (possibly formed by the fibroblasts).
It differs from the white fibrous tissue in the following respects:
i. It has got a yellowish colour.
ii. The fibres are thicker.
iii. The individual fibres branch freely and the branches join with one another to form a network.
iv. The fibres may run singly as well as in small loose bundles. Even in the bundle the outlines of the fibres are clearly visible
v. The bundles are not wavy but follow a straight course.
vi. When the fibres are torn by stretching, the broken ends quickly curl up due to elastic recoil.
vii. In transverse section the fibres appear to be angular with the angles rounded off.
viii. Elastic fibres are composed of a protein, elastin, which is resistant to most chemical agents but is digested by pancreatin.
Distribution:
It is found in the areolar tissue throughout the body. It is present in the hollow viscera where the restoration of normal configuration is essentially required. It is found in the most concentrated form in the ligamentum nuchae of the quadrupeds, in the ligamentum flava of the vertebra.
It is also found in the walls of the bronchi and in the larynx, uniting the cartilages. It is also present in the lungs and in the walls of the arteries and in one form of fibrocartilage. Elastic tissue does not always remain in the form of fibres and bundles but may also occur as a continuous membranous sheath, such as the internal elastic lamina of the blood vessels.
Functions:
The function of the elastic tissue is always due to its strength, extensibility and elastic recoil. In other words, it serves the purpose of a strong elastic rope.
i. In the form of ligaments it holds the connected parts firmly together and at the same time allows considerable latitude of movement.
ii. In blood vessels it prevents excessive dilatation and by its elastic recoil serves to maintain circulation and blood pressure.
iii. In the lungs its elastic recoil helps expiration as well as maintains and adjusts the negative pressure in the pleura.
5. Reticular Tissue (Fig. 1.40):
Description:
It is similar to the areolar tissue with certain peculiarities.
The reticular fibres here resemble white fibrous tissue, having the following differences:
i. They are thinner, freely branching and resist peptic digestion.
ii. They are selectively stained by silver oxide or carbonate solution. Hence called argyrophil fibres.
Interspaces are very small and are largely occupied by lymph and tissue fluid. The cells of this tissue belong to the so-called reticuloendothelial system. Reticular tissue is widely distributed. It forms the basement membrane of many epithelia, the framework of many organs, supporting their essential cellular elements.
Function:
It occurs in lymph nodes, liver, spleen, bone marrow and many other organs.
6. Blood and Haemopoietic Tissue:
Blood cells are also considered to be the special type of connective tissue and have been dealt in detail in the section of blood.
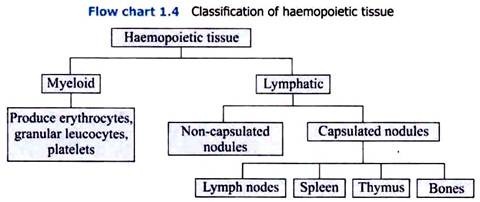
Haemopoietic (properly haemocytopoietic) tissues are of two types (Refer flow chart 1.4):
i. Myeloid.
ii. Lymphatic.
Lymphatic tissue generally gives rise to lymphocyte, and myeloid tissue normally produces erythrocytes, granular leucocytes, and platelets. Monocytes are produced from both the tissues.
i. Myeloid Tissue:
It has got both phagocytic as well as blood cell-producing functions. It produces erythrocytes, granular leucocytes and platelets. Myelos means marrow. Normally the term myeloid tissue and bone marrow are used synonymously.
ii. Lymphatic Tissue:
The lymphatic tissue can be subdivided under the following:
i. Non-capsulated nodules of lymphatic tissue in the loose connective tissue.
ii. Capsulated lymphatic tissues which are present in specific lymphoid organs, viz., lymph node or lymph gland, Spleen, thymus tonsil.
7. Cartilage:
It is a connective tissue which is more or less translucent, firm in texture and to some extent elastic. In firmness and elasticity it occupies a position intermediate between fibrous tissue and bone. It is made up of cartilage cells, chondroblasts and a large amount of intercellular ground substance (matrix), constituted by the fibres and two types of proteins—chondromucoid and chondroalbumoid (chondroalbuminoid).
On hydrolysis, the former gives chondroitin sulphuric acid. The ground substance either may be clear and homogeneous or may contain fibrous tissue. These fibres may be either white fibrous tissue or yellow elastic tissue.
Functions of Cartilages:
In elasticity and hardness cartilages stand midway between fibrous tissue and bone.
Hence, their main function is:
i. Mechanical:
It helps to maintain shape and rigidity of structure combined with certain amount of elasticity. This is well seen in the costal cartilages. It also acts as a mechanical buffer as found in the intervertebral discs, articular menisci, etc.
ii. Hyaline Cartilage:
Hyaline cartilage serves also the very important function of forming the primary medium in which cartilaginous development of bone takes place. Fibrous cartilage acts as strong, flexible connecting substance between bones. Elastic cartilage maintains and strengthens the attached organs.
8. Jelly-Like Connective Tissue:
This may be described as an embryonic form of areolar tissue in which deposition of fibrous tissue has not yet taken place and the cells remain scattered in a more or less homogenous jelly-like ground substance and with few fibres interlacing throughout the tissue.
The cells are large fibroblasts with a few macrophages and lymphocytes, the ground substance being mucin in nature. The tissue occurs in the umbilical cord where it is known Wharton’s jelly. In adult life it is found to compose the vitreous humour in the eyeball.
9. Osseous Tissue or Bone:
This tissue which constitutes the skeleton is the hardest of all connective tissues. It is made up of bone cells and intercellular ground substance. The organic part of the latter which is about 40 percent is composed of collagen fibres, the osteocollage- nous fibres, and is bound by a mucopolysaccharide cementing material (ossein). The remaining 60 percent which is deposited as a dense substance is inorganic, mainly calcium salt (vide later). Bone is covered with periosteum (around bone).
Bone Marrow:
The central marrow cavities of long bones and between the spicules of latticework of spongy bones are filled with bone marrow. When the osteoblasts invade the cartilage model, marrow begins to form in it.
Yellow marrow is composed mainly of fat cells or adipose tissue and is found in the marrow cavity of long bones, whereas red marrow is associated with spongy bones, and contains a certain amount of adipose tissue and mostly blood-forming tissue.
Functions:
i. Production of blood cells and their release in circulation.
ii. Erythroclasia.
iii. Reticulo-endothelial functions.
iv. Osteogenic functions.
v. Immunologic functions.
vi. General connective tissue functions.
Blood Vessels, Lymphatics and Nerves of Bone:
The nutrient artery by means of the medullary or nutrient canal near the centre of shaft (diaphysis) supplies blood vessels to the long bone. After piercing the compact bone the nutrient artery branches to the vessels in the Haversian canals. Then after reaching the central marrow cavity, this artery is divided into a descending and an ascending branch and these branches, being broken up into a capillary network, supply all the marrow.
Besides this, the periosteum collects blood vessels in the bone. Communicating canals (Volkmann’s canals), after piercing the bone, supply blood vessels through the Haversian canals of compact bone or through the marrow spaces of spongy bone. From the Haversian canals, the vessels extend branches into the marrow cavity and their capillaries anastomose with other group of arteries.
The Haversian canals collect blood capillaries through thin-walled valveless veins and ultimately these capillaries reach periosteum again through the communicating canals (Volk- mann’s canals) or through the nutrient canal. According to some, lymphatics occur in the compact bone and others describe them in the periosteum. Both myelinated and non-myelinated nerve fibres, accompanying blood vessels in the canals, are found in the periosteum. But myelinated nerves are numerous in the bone marrow.
Studies of refractive indices, X-ray diffraction pattern, etc., indicate that calcium phosphate and calcium carbonate do not remain separately. It is shown that bone is crystalline in structure and that the calcium salts remain combined together to form bigger compounds belonging to the ‘apatite class’. Some hold that CaHPO4 is possibly formed first, which is then converted into other compounds. Anyway Ca3 (PO4)2 is the chief final compound, which remains attached to CaCO3 mainly and to some extent to CaHPO4 and Ca(OH)2.
Bone calcium is not a static material. Experiments with radio-active isotopic calcium (45Ca) shows that it is in constant exchange with the body fluids and thus maintains s dynamic equilibrium. If calcium salts with radio-active calcium be given intravenously, 86% of it is taken up by bone in 100 min.
About 10% of is replaced in 10 days and the whole of it in 200 days. This possibly shows that the entire calcium content of bones is renewed every 200 days. Lead, other toxic elements, and also radio-active strontium which is produced from explosion of atom bomb, are taken up by bone similar to calcium. Due to radiation, uptake of latter is harmful.
10. Reticulo-Endothelial Tissue:
This possesses various types of connective tissue cells which are widely distributed in the body, the phagocytic cells which are found mainly in bone marrow, liver capillaries, lymph nodes, serous membranes, splenic sinusoids.
Function:
These cells are important for defence of body against foreign particulate substance and micro-organism.