The following points highlight the five major types of neuropsychiatric disorder. The types are: 1. Myasthenia Gravis at the Neuromuscular Junction 2. Huntington’s Disease 3. Parkinson’s Disease 4. Alzheimer’s Disease 5. Schizophrenia.
Neuropsychiatric Disorder: Type # 1. Myasthenia Gravis at the Neuromuscular Junction:
a. The recurrent episodes of muscle weakness produce Myasthenia Gravis.
This is improved by administration of drugs that inhibit acetyl-cholinesterase.
b. The body forms autoantibodies against the acute acetylcholine receptor (ACHR) of the neuromuscular junction. These antibodies destruct the receptors.
c. The neuromuscular junction consists of a single nerve terminal separated from the postsynaptic region by the synaptic clefts.
The overall process at the junction takes place in six steps:
(i) In the cytosol of the nerve terminal, acetylcholine is synthesized by the enzyme choline acetyltransferase.
Acetyl -CoA + choline → Acetylcholine + CoA
(ii) Acetylcholine is then incorporated into synaptic vesicles and stored therein.
(iii) Acetylcholine is released from these vesicles into the synaptic cleft.
(iv) The released one diffuses rapidly across the synaptic cleft to its receptors in the junctional folds.
(v) The acetylcholine is then hydrolysed by acetyl-cholinesterase in the following manner.
Acetylcholine + H2O → Acetyl + Choline
(vi) The choline is recycled into the nerve terminal by the active transport mechanism.
Inhibitors of Cholinesterase for the Treatment of Myasthenia Gravis:
a. There are two types of inhibitors of cholinesterase reversible and irreversible. Both are short-acting and long-acting reversible inhibitors. The former is mostly used in diagnosis. The diagnosis depends on history, clinical findings, and laboratory tests.
b. Pyridostigmine and nesotigmine are the effective agents for the treatment of this disease.
c. Disopropylflurophosphate (DFP) binds to a serine residue in the active centre of acetyl cholinesterase. It is the toxic nerve gas and is also used as an insecticide.
d. Severe cases may require administration of azathioprine.
Neuropsychiatric Disorder: Type # 2. Huntington’s Disease:
a. This is an inherited disease in an autosomal dominant manner. Fifty percent of the children of an affected parent are at risk. It usually begins between 35 and 50 years of age and the duration is 15 years after onset.
b. This disease affects the neurons in the corpus striatum. Many die and are partly replaced by glial cells.
c. The levels of some neurotransmitters (e.g., GABA) and acetylcholine of some enzymes involved in their synthesis are decreased.
d. The levels of dopamine and norepinephrine are increased.
Neuronal Death in Huntington’s Disease:
a. This disease is characterized by the death of certain neuron due to certain chemicals (excitotoxins) which may be exogenous or endogenous.
b. Glutamate and aspartate are excitatory amino acids in the brain. Glutamate receptors have been subdivided into five classes.
c. The NMDA (N-methyl-D-aspartate) receptor plays a central role in long-term potentiation which results in an increase of synaptic efficacy in the hippocampus and other areas and may be involved in memory and learning.
Excitotoxins & Other Biochemical Mechanisms are Involved in Brain Damage due to Store:
a. In a stroke,brain damage occurs due to diminished blood flow. Strokes are the third leading cause of death.
b. Most strokes are caused by thromboses in the cerebral arteries. This reduces the supply of oxygen and glucose to the brain.
c. Ischemia causes depolarization of the neuronal membrane, leading to release of glutamate which stimulates the AMPA.
d. Increased intracellular Na+ activates Na+/Ca++ transporters. Voltage gated Ca++ channels are activated by depolarization. Inositol triphosphate releases Ca++ which releases additional glutamate for exciting neighbour neurons.
e. The high level of intracellular activates Ca++dependent nucleases, Proteases and phospholipases. Degradation of phospholipids can also lead to formation of platelet -activating factor (PAF) and release of arachidonic acid which forms eieosanoids.
f. The disease may be prevented by treatment of risk factors such as hypertension, diabetes mellitus, smoking and hyperlipidemia. Low dose aspirin therapy is effective in lowering the risk of stroke.
Neuropsychiatric Disorder: Type # 3. Parkinson’s Disease:
Parkinson’s Disease Reflects a Deficiency of Dopamine:
a. Parkinson disease is characterized by tremor, bradykinesia, rigidity and postural instability. It U-rarely occurs before 40 years of age.
b. The pathologic characteristic of the disease is degeneration of the pigmented cells in the substantia nigra. When normal, these cells synthesize and use dopamine as a neurotransmitter and thus are said to be dopaminergic.
c. There is no evidence for a significant genetic component in this disease.
The cell damage may reflect the process of ageing.
d. Viral infections can cause this disease. Drugs are important causes of Parkinsonism which can be reversible when therapy is stopped.
e. Mazindoi inhibits the uptake of dopamine increasing the concentration of dopamine at the postsynaptic junction.
f. Surgical treatment includes the injection of minced adrenal auto grafts,
g. The antiviral agent amantadine induces release of dopamine from the presynaptic terminals of dopaminergic cells.
Neuropsychiatric Disorder: Type # 4. Alzheimer’s Disease:
a. It is an uncurable neuropsychiatric condition and its prevalence increases as more people live longer.
b. This disease is the commonest cause of dementia which ensures the decline in intellectual functions due to an organic cause. It imposes a heavy burden on families and on health care system and most patients cannot look after themselves.
c. The usual age in the starting of this disease is over 65 years, but it can occur at the age of 40 also. The survival period ranges from 2 to 20 years. The first symptom is the loss of memory.
d. The pathologic finding is characterized by the loss of cells in certain areas of the brain. Deposits of amyloid are common in small blood vessels.
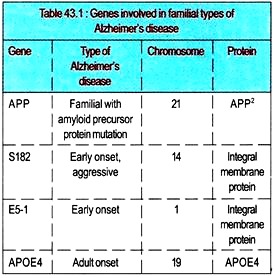
e. Amyloid p protein, the major constituent of the plaques is present in this disease. Amyloid is a group of extracellular protein deposits found in many different diseases. Amyloid proteins stain blue with iodine. AβP is derived from a larger precursor protein named amyloid precursor protein (APP) whose gene is located on chromosome 21 close to the area affected in Down’s syndrome. Patients with Down’s syndrome who survive till age 50 often suffer from Alzheimer’s disease.
f. APP is a protein of 770 amino acids and AβP is a peptide of 39-42 amino acids derived from AβP by proteolytic cleavage.
g. One of the genes of Alzheimer’s disease is encoded by APP and the mutations in this gene can lead to the increased deposition of AβP in neurons.
h. AβP-containing fragments is directly or indirectly neurotoxic. Some protein kinases are regulated by levels of Ca2+.
i. Recently, two genes have been isolated in connection with Alzheimer’s disease which encode trans membrane proteins and show homology to the SPE-4 protein of caenorhalditis elegans. The protein participate in the fibrous body membrane organelle (FBMO) complex during spermatogenesis. The FBMO plays a role in the transport of soluble membrane bound proteins.
Role of other Factors in Alzheimer’s Disease:
i. Infection with a slow virus is the cause of the disease although no such virus has been isolated.
ii. Another finding shows that plaques from patients with this disease often contain large amounts of aluminium.
iii. The brains of patients who have died from Alzheimer’s disease often show a marked reduction in choline acetyltransferase and acetylcholine. The levels of other neurotransmitters are also decreased.
iv. The levels of APP become lower in the cerebrospinal fluid of patients with Alzheimer’s disease.
v. It has become possible to change the deposition of AβP in tissues by drugs although
no specific drug therapy for Alzheimer’s disease is yet available.
Neuropsychiatric Disorder: Type # 5. Schizophrenia:
Causes of Schizophrenia:
a. The schizophrenic disorders are mental disorders characterized by psychotic symptoms having disturbances of thinking, feeling, and behaviour. There are a number of subtypes, e.g., disorganized, catatonic, and paranoid.
b. This disorder starts before the age of 45 and turns to a chronic course. It is a major medical problem with devastating consequences for the victim and family members.
c. The causes of schizophrenia are unknown. Various psychologic, social, developmental, environmental, anatomic, genetic, biochemical and other factors are involved.
Schizophrenia due of Lack of Replication:
a. A child born to parents both of whom are schizophrenic has a 39 per cent chance of developing the condition.
b. A disease occurs in a family does not mean that it has a genetic origin. Poor psychologic interactions among family members can lead to abnormal behaviour patterns.
c. It has multiple genetic causes.
Dopamine has been Implicated in Schizophrenia:
a. Acetylcholine, GABA, norepinephrine, peptides, and other molecules are involved in the causation of this disorder.
b. Neuroleptic drugs are acting to lower levels of dopamine. Neuroleptics act primarily by reducing dopamine activity in mesolimbic dopamine neurons.
c. There is the increase in the amounts of dopamine in brain tissue samples of patients with schizophrenia as per the reports of a number of observers.
d. Prolonged treatment with neuroleptics leads to a fall in the levels of homovanillic acid in cerebrospinal fluid.
e. The antipsychotic potencies of most neuroleptics correlate with their binding to D2 receptors.
f. All of the five classes of receptors are trans-membrane proteins, some are glycoproteins, and most appear to be coupled to G proteins. D4 is the first receptor in the catecholamine family.
g. On the basis of analysis of postmortem specimens, it has been found that the density of D2 receptor is increased in the brains of schizophrenics.
h. The low dopamine activity in the prefrontal cortex shows negative symptoms of schizophrenia.