The below mentioned article provides a short note on Meningitis.
Introduction:
Leptomeningitis is an inflammation of the membranes surrounding the brain and spinal cord (para-arachnoid). It may be caused by viruses, bacteria, fungi and protozoa. Infection may occur either through the blood (blood borne) or by direct spread along sinuses and veins from other parts of the body.
Acute pyogenic meningitis may be caused by pyogenic organisms and tuberculous meningitis by M. tuberculosis.
Acute Pyogenic Meningitis:
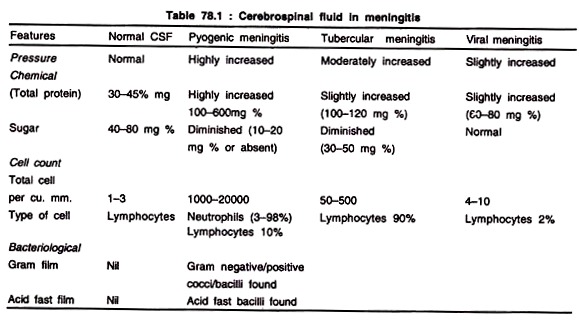
Diagnosis of acute pyogenic meningitis is done by the direct examination of cerebrospinal fluid (CSF). A clear indication of the causal organisms of meningitis can be obtained by chemical and cytological examination of CSF (Table).
The CSF usually contains more than 1,000 leukocytes per cu. mm, 90-95% of which are polymorphonuclear leukocytes. The protein content is elevated, often more than 100 mg % and the glucose level is markedly diminished Or even absent.
A. Causative Organism:
1. N. meningitidis
2. Str. pneumoniae
3. H. influenzae
4. Staph, aureus
5. Listeria monocytogenes
6. Gram positive/negative organisms
7. E.coli, Proteus, Klebsiella, Citrobacter, Enterobacter, Serratia. R.
B. In Neonates:
1. E.coli
2. Str. agalactiae group B
3. L. monocytogenes
4. Klebsiella
The incidence of various types of meningitis varies greatly with the age of the patient. E.coli, Str. haemolyticus group B and Staph, aureus are important causes in infants of first few months. Meningitis due to H. influenza is common between 3 months to 5 years of age. Meningococcal and pneumococcal meningitis can occur at any age.
Infection due to L.monocytogenes is found in neonates and immuno-compromised host. Certain fungi (Cryptococcus neoformans, Histoplasma capsulatum, Coccidioides immitis, Candida albicans and Aspergillus) may occasionally cause meningitis. They are found in immuno-compromised patients (e.g. those with leukemia, lymphoma, AIDS or on immuno-suppressive drug).
Laboratory Diagnosis:
CSF is obtained by lumbar puncture. The fluid should be examined immediately after collection. The fluid is collected in 3 separate sterile vials — one for cell count; one for chemical examination and one for culture. The type of meningitis can be indicated by routine chemical examination and cell count.
A. Microscopy:
Microscopy examination of smear made from centrifuged deposit will show plenty of pus cells and few Gram-negative or Gram-positive bacteria.
B. Culture:
1. CSF Blood agar, Chocolate agar, and cooked meat medium are inoculated with the centrifuged deposit and incubated for 24 hours in 5-10% CO2.
The isolates were identified by biochemical and serological test.
2. Blood. Blood culture is useful and may be positive in about 50% of cases of meningitis due to N. meningitidis, H. influenzae and Str. pneumoniae.
C. Demonstration of Bacterial Products:
1. Bacterial antigens can be detected by immunological test (latex agglutination) counter current Immunoelectrophoresis. (CIEP) and ELISA using specific antisera to common sero group A, C of N. meningitidis, H. influenzae and Str. pneumoniae.
2. Bacterial Endotoxins:
The limulus lysate test is specific and sensitive for the detection of bacterial endotoxin.
Tubercular Meningitis:
In this infection CSF shows moderate rise in:
(a) Cell count (50-500 per cu.mm) — most of them are lymphocytes.
(b) Protein (80-120 mg %).
(c) Sugar is diminished (30-50 mg %).
Ziehl-Neelsen stained smear of centrifuged deposit reveals few lymphocytes with few M. tuberculosis.
Culture:
After inoculation of centrifuged deposit of urine on L-J medium and incubation for 6-8 weeks, M. tuberculosis colony is formed.