The normal kidney has tremendous capability to vary the relative proportions of solutes and water in the urine. They can excrete urine with an osmolarity as low as 50 mOsm/L, when there is excess water in the body and ECF osmolarity low. They can also excrete urine with a concentration of 1200-1400 mOsm/L, when there is a deficit of water and extracellular fluid osmolarity high.
Obligatory Urine Volume (OUV):
The maximal concentrating ability of the kidney depends on how much urine volume must be excreted each day, to void the body of waste products of metabolism and ions that are ingested. A normal 70 kg human must excrete about 600 mOsm of solute each day.
If maximum urine concentrating ability is 1200 mOsm/L, the minimal volume of urine is OUV can be calculated as:
(600 mOsm/day)/(1200 mOsm/L) = 0.5 L/day
Requirements for Excreting Concentrated Urine:
1. High ADH levels.
2. Hyperosmotic renal medulla.
1. High ADH Levels:
When osmolarity of the body fluids increases above normal the posterior pituitary secretes more ADH.
This increases the permeability of the distal tubule and collecting duct to water. So, more water is reabsorbed and concentrated urine is formed.
When there is excess water and ECF osmolarity is reduced, ADH from posterior pituitary decreases, thereby reducing permeability of distal tubule and collecting duct to water causing dilute urine.
Hyperosmotic Renal Medulla:
Hyperosmotic renal medulla is produced by counter-current mechanism and urea.
The renal medullary interstitium surrounding the collecting duct is very hyperosmotic. So, when ADH levels are high, the water moves through the tubular membrane by osmosis into the renal interstitium, from there into vasa recta back into blood.
The countercurrent mechanism depends on the special anatomical arrangement of the long loops of Henle of juxtamedullary nephrons and the vasa recta, the specialized peritubular capillaries of the renal medulla. Loop of Henle is called as countercurrent multiplier and vasa recta as countercurrent exchanger.
The corrected osmolar activity which accounts for intermolecular attraction and repulsion is about 282 mOsm/L. The osmolarity of renal interstitium is about 1200 to 1400 mOsm/L in the tip of medulla.
The major factors that contribute to high solute concentration into the renal medulla are:
1. Active transport of sodium ions and cotransport of potassium chloride out of the thick ascending limb of LOH into medullary interstitium.
2. Active transport of ions from the collecting ducts into the medullary interstitium.
3. Passive diffusion of large amounts of urea from inner medullary CD into the medullary interstitium.
4. Diffusion of only small amounts of water from tubules into interstitium.
Countercurrent Multiplier System in the Loop of Henle (Fig. 8.24):
Step 1:
Assume the loop of Henle (LOH) is filled with fluid with a concentration of 300 mOsm/L, the same concentration as in proximal tubule.
Step 2:
The active transport of Na+ and other ions out of thick ascending limb of LOH reduces the concentration of solute inside tubule but raising in interstitium.
Step 3:
The tubular fluid in the descending limb of LOH and interstitium reaches osmotic equilibrium because of osmosis of water out of descending limb. The osmolarity in interstitium maintained at 400 mOsm/L.
Step 4:
It is additional flow of fluid into LOH from proximal tubule which causes hyperosmotic fluid in descending limb to move into ascending limb.
Step 5:
When fluid is in ascending limb, additional ions are pumped into interstitium with water remaining behind until a 200 mOsm/L osmotic gradient is reached, with interstitium fluid osmolarity raising to 500 mOsm/L.
Step 6:
Once again the fluid in descending limb reaches equilibrium with hyperosmotic interstitial fluid. This fluid moves from descending limb to ascending limb so more solute is pumped out of the tubules and deposited in interstitium. These steps are repeated again and again till interstitium osmolarity reaches 1200-1400 mOsm/L.
Urea Contribution to Hyperosmotic Renal Medullary Interstitium (Fig. 8.25):
Urea contributes about 40% (500 mOsm/L) of osmolarity of the renal medullary interstitium. When there is water deficit and ADH levels in blood are high, large amounts of urea are passively released from inner medullary collecting duct into interstitium which is highly permeable to urea.
Urea can also be re-circulated from collecting duct into interstitium. The thick ascending limb of LOH, distal tubule and cortical collecting duct are impermeable to urea. A person usually excretes 40-60% of filtered urea.
Excretion depends on two factors:
a. Concentration of urea in plasma.
b. GFR.
Countercurrent Exchange in the Vasa Recta Preserves Hyperosmolarity (Fig. 8.26):
The vasa recta are highly permeable to solutes in the blood, except for the plasma proteins. Plasma flowing down the descending limb of vasa recta becomes more hyperosmotic because of diffusion of solutes from interstitial fluid into blood. In the ascending limb LOH, solutes diffuse back into interstitial fluid and water diffuses back into vasa recta.
Osmolar Clearance (Cosm):
It is the volume of plasma cleared of solutes each minute. It is expressed in ml/min.
Cosm = Uosm × V/Posm
Uosm is urine osmalarity. V is urine flow rate. Posm is plasma osmolarity.
Free Water Clearance (CH2O):
The rate at which solute-free water is excreted by the kidneys. It is expressed in ml/min.
CH2O = V – Cosm = V – (Uosm x V)/Posm
It is calculated as the difference between urine flow rate and osmolar clearance. When CH2O is positive, excess water is being excreted by kidney. When CH2O is negative excess solutes are being removed from the blood by kidneys.
Disorders of Urine Concentrating Ability:
It can be due to:
1. Inappropriate secretion of ADH as in central diabetes insipidus, cause being congenital infections or head injuries.
2. Impairment of countercurrent mechanisms.
3. Inability of DT, CD to respond to ADH. In conditions like nephrogenic diabetes insipidus and in usage of various drugs like lithium and tetracyclines, even if ADH is produced in normal amounts, abnormality of kidneys makes them to fail to respond to ADH.
Formation of Urine—Glomerular Filtration:
The rate at which different subs the urine represents the sum of three renal processes:
1. Glomerular filtration.
2. Tubular reabsorption of substances from the renal tubules into the blood.
3. Tubular secretion of substances from the blood into renal tubules.
Excretion = Filtration – Reabsorption + Secretion
Urine Formation Renal Handling of Substances:
Four classes of substances:
a. Filtered, not reabsorbed (creatinine, inulin, uric acid).
b. Filtered, partly reabsorbed (Na+, CI–, bicarbonate).
c. Filtered, totally reabsorbed (amino acids, glucose).
d. Filtered, totally secreted (organic acids and bases).
Glomerular Filtration (Fig. 8.13):
It is the first step in urine formation.
Glomerular filtrate is produced from blood plasma. It must pass through the glomerular membrane which is relatively impermeable to proteins. So the filtrate is similar to plasma in terms of concentrations of salts and of organic molecules (e.g., glucose, amino acids) except it is essentially protein-free and devoid of cellular elements including red blood cells.
Formation of Urine—Tubular Reabsorption and Tubular Secretion:
Introduction:
Tubular reabsorption and tubular secretion are selective and quantitatively large. It includes both passive and active transport mechanisms. Water and solutes can be transported through all membranes themselves (transcellular route) or through the junctional spaces between the cells (paracellular route). From the cells into interstitial fluid, water and solutes are transported by ultrafiltration (bulk flow) mediated by hydrostatic and colloid osmotic forces.
Tubular Reabsorption:
1. Sodium:
Potassium ATPase, hydrogen ATPase, hydrogen-potassium ATPase and calcium ATPase are examples of primary active transport. It moves solutes against an electrochemical gradient. The energy is provided by the membrane bound ATPase.
In secondary active co-transport of glucose and amino acids, sodium diffuses down its electrochemical gradient; the energy released is used to drive another substance that is glucose/amino acid.
2. Secondary Active Counter Transport:
Sodium hydrogen counters transport. The energy liberated from the downhill of one of the substances (e.g., sodium) enables uphill of a second substance (hydrogen) in the opposite direction.
3. Pinocytosis:
Reabsorption of proteins occurs by this process. In this, protein gets attached to the brush border of the luminal membrane which invaginates into the interior of the cell until it completely pinches off and a vesicle is formed.
Solvent Drag:
As water moves across the tight junctions by osmosis, it can also carry with it some of the solutes a process called solvent drag.
Transport Maximum (Tm):
Transport maximum (Tm) for substances that are actively; reabsorbed or secreted. There is a limit to the rate at which the solute can be transported, termed as transport maximum. This is due to the saturation of the specific transport systems involved when the tubular load of solutes exceed the capacity of the carrier proteins involved in the transport process.
There is a relation between tubular load of glucose, Tm for glucose and rate of glucose loss in the urine, when tubular load is 125 mg/min, there is no loss of glucose in urine. When tubular load rises above 180 mg/min, a small amount appears in the urine that is called renal threshold for glucose. This appearance of glucose occurs even before Tm is reached. The reason being not all nephrons have same Tm for glucose.
Splay:
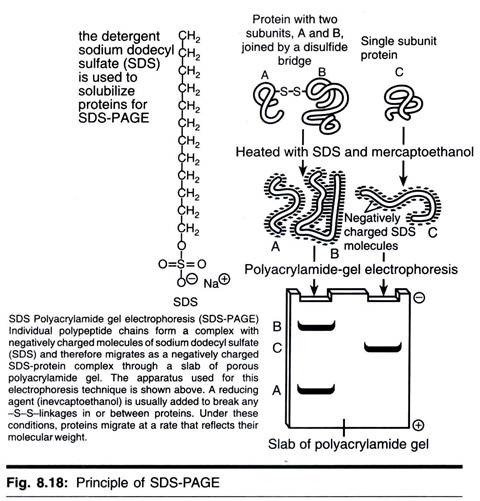
The ideal curve shown in this diagram (Fig. 8.18) is obtained if the TmG in all the tubules was identical. This is not the case in humans, the actual curve is rounded and deviates from the ideal curve. This deviation is called splay. The magnitude of the splay is inversely proportionate to the avidity with which the transport mechanism binds the substance it transports. Tm for actively secreted substances.
For example:
Creatinine: 16 mg/min
PAH: 80 mg/min
Gradient Time Transport:
It is for passively reabsorbed substances which depend on the electrochemical gradient and the time that the substance is in the tubule which in turn depends on the tubular flow rate.
Regulation of Tubular Reabsorption:
Nervous:
Sympathetic nervous system stimulation decreases.
a. Sodium and water excretion by constricting the renal arterioles.
b. Increase Na reabsorption in proximal tubule and thick ascending limb of LOH.
c. Increases renin and angiotensin II release.
1. Hormonal:
Hormones that regulate tubular reabsorption:
a. Aldosterone:
Site of action ― Collecting duct.
Effects ― Increases NaCl, H2O reabsorption increases K+ secrection.
b. Angiotensin II:
Site of action ― Proximal convoluted tubule, thick ascending limb of loop of Henle.
Effects ― Increases Nacl, H2O reabsorption and H+ secrection
c. ADH:
Site of action ― Distal tubule/Collecting duct
Effects ― Increases H2O reabsorption
d. ANP:
Site of action ― Distal tubule/Collecting duct
Effects ― Increases NaCl reabsorption
e. Parathormone:
Site of action ― Proximal tubule, thick ascending limb, distal tubule
Effects ― Decrease PO4– reabsorption in proximal tubule
Increases Ca++ release in loop of Henle
Increases Mg+ reabsorption in loop of Henle
2. Local Control:
a. Glomerulotubular balance: Increased GFR increases the tubular load thereby increasing tubular reabsorption.
b. Peritubular capillary and renal interstitial forces. Reabsorption = Kf × Net reabsorption force (NRF).
The NRF represents the sum of hydrostatic and colloid osmotic forces which favor or oppose reabsorption across peritubular capillaries.
These forces are (Fig. 8.19):
a. Peritubular hydrostatic (Pc) pressures oppose RA = 13 mm Hg.
b. Renal interstitial hydrostatic (Pif) favoring RA = 6 mm Hg.
c. Colloid osmotic pressure in peritubular capillaries favors RA (C) = 32 mm Hg.
d. Colloid osmotic pressure in renal interstitium opposes RA (if) = 15 mm Hg.
Proximal Convoluted Tubules:
i. Reabsorbs 65% of glomerular filtrate by active transport.
ii. Reabsorbs Na+, CP, HCO3, K+, Ca+, H2O, glucose, amino acids, vitamins, uric acid and phosphates. Pars recta secretes substances like creatinine, phenolphthalein dyes, PAH, acids, bases, drugs like penicillin, sulphonamides.
Loop of Henle:
Descending thin segment is highly permeable to water. Water moves out of nephron reducing the volume of filtrate and increasing its osmolarity.
Ascending thick segment is not permeable to water but is permeable to solutes. 25% of filtered solutes are reabsorbed.
Distal Tubule (Fig. 8.20):
The very first portion of the distal tubule forms part of JG apparatus. The next early part is highly convoluted and has same re-absorptive characteristics as that of ascending limb of loop of Henle. Na+, Cl– H2O, HCO3, Ca+ and K+ are reabsorbed but impermeable to water and urea. This is also known as diluting segment because it dilutes the tubular fluid.
Collecting Tubule:
The second part of the distal tubule is the late distal tubule continues as cortical collecting tubule having principal cells and intercalated cells. The tubular membranes are impermeable to urea is concerned with Na+, CI– reabsorption, HCO3 secretion, HCO3 reabsorption, secretion of K+ and H+ secretion. The permeability of the tubules to water is controlled by antidiuretic hormone (ADH) (Fig. 8.21). 
Medullary Collecting Duct:
They are the final site for processing urine. The permeability to water depends on presence of ADH. They are permeable to urea and secrete H+ against a large concentration gradient. 15% of solutes are reabsorbed in distal tubule and collecting duct.
Sodium and Chloride Reabsorption:
Na+ is reabsorbed in PCT, thick segment of LOH and distal nephron except in thin segment.
Mechanisms:
In PCT: 65-70%
Unidirectional Na Transport:
Movement of Na+ against concentration gradient-glucose, amino acids and phosphate are transported with it.
Na+ — H+ exchange (antiport)
In thick ascending limb-25%:
1 Na+— 1 K+ — 2 CI– symporter.
Distal Nephron-10%:
Unidirectional Na+ transport but under the influence of aldosterone.
Glucose and Amino Acid Reabsorption:
i. Reabsorbed in PCT.
ii. Na+ cotransport mechanism.
Sodium dependent glucose transporter (SGLT) on luminal (apical) membrane and glucose transporter on the basolateral membrane (GLUT).
Water Reabsoption:
i. PCT:
65 to 70%
Passive transport by osmosis (couples to Na reabsorption).
Solvent drag through paracellular route—water takes Na+, CI–, K+, Ca+, Mg+ along with it. As the substances are absorbed proportionally, the fluid remains isotonic at the end of PCT. This passive reabsorption of water is called obligatory type of reabsorption.
ii. DT and CD:
Under ADH control.
ADH introduces water channels called aquaporins which allows water absorption. Water is absorbed from collecting duct only in the presence of ADH. This is called facultative type of reabsorption.
Potassium and Reabsorption Secretion (Fig. 8.21):
In PCT- Solvent drag through paracellular route causes K+ reabsorption.
Minimal secretion of K+ occurs through the luminal membrane.
In Thick Ascending Limb:
1 Na+ — 1 K + 2 Cl– co-transporter causes reabsorption.
In late distal tubule and collecting duct, P cells, reabsorb Na+ and secrete K+. I cells reabsorb K+ and HCO3, secretes H+ ions.
Hydrogen Ion Secretion (Figs 8.22 and 8.23):
i. In PCT
ii. In DT and CD
a. Intercalated cells secrete H+ ions
b. H+ ATPase (primary active transport).