In this article we will discuss about the composition and enzymes of gastric juice.
Composition of Gastric Juice:
i. Gastric juice is the secretion of gastric glands.
ii. Total amount secreted: 1, 200-1.500 ml per day.
iii. Night secretion (during sleep) alone is 400 ml/day.
iv. Acidity of gastric juice: 40-60 mEq/liter
v. pH: 0.9-1.5
vi. Water content—99.45%
vii. Total solids—0.55%
viii. Specific gravity—1.002-1.004
ix. Solids: Inorganic: 0.15% (NaCl, KCl, CaCl, calcium phosphate, magnesium phosphate, bicarbonate, etc.)
x. Organic: 0.4%
a. Mucin, blood group, substances, intrinsic factor of castle
b. Enzymes: Pepsinogen, gastric lipase, rennin (absent in adult human beings, may be present in infants)
xi. Characteristic component of gastric juice is HCl.
Enzymes of Gastric Juice:
Pepsinogens:
Three different pepsinogens have been discovered. Pepsinogen I, II and III. Molecular weight is about 46,000.
i. Pepsinogen is activated by HCl to pepsin; pepsin itself can cause activation of pepsinogen (auto- catalysis). Activation involves only the removal of a short peptide from pepsinogen.
ii. Molecular weight of pepsin: 35,000
iii. Pepsin acts at pH of 1.5-3.5
iv. Being a proteolytic enzyme, it converts larger proteins into smaller polypeptides by attaching peptide bonds involving phenylalanine or tyrosine.
v. A small amount of pepsin is excreted in urine as uropepsin.
vi. Rennin If present has got an action on milk by clotting it. This is nothing but conversion of soluble caseinogen into insoluble calcium caseinate. Since rennin is mostly absent in human beings, pepsin performs the same action.
vii. Gelatinase: It is a very useful enzyme for the digestion of gelatin. The gastric enzymes are not essential for life. Most important gastric enzyme is pepsin and what pepsin can do; the pancreatic trypsin does equally well.
viii. Gastric mucins: There are two types of mucin. Soluble mucin from the mucous neck cells and the insoluble mucin from the surface epithelium of stomach.
Functions of Mucin:
a. Mucin along with the bicarbonate protects the gastric walls from the action of gastric HCl and pepsin.
b. The mucin lining the mucous membrane of the stomach forms a mechanical barrier preventing HCl and pepsin to come in contact with gastric mucosa. A breakdown of this barrier can easily result in formation of peptic ulcers.
Peptic ulcers can be defined as ulcers in the gastric wall caused by acid peptic digestion. (Ulcers in general mean a discontinuity in skin or mucous membrane.)
Nowadays, it is be believed that more than the mucin barrier, the very structure of gastric mucous membrane with its tight intercellular junctions forms a more effective barrier to the action of HCl and pepsin. Gastric mucin secretion is stimulated by any type of chemical or mechanical irritation of the stomach. The drug aspirin, alcohol, etc., can break the mucin barrier and increase the susceptibility (vulnerability) to peptic ulcer.
Functions of HCI:
a. Activation of pepsinogen to pepsin.
b. Provides an acid medium for the action of pepsin.
c. Being a strong acid, it can kill many bacteria that have entered stomach along with the food.
d. HCI in the duodenum can stimulate and increase the secretion of bile from liver and the exocrine secretion from pancreas.
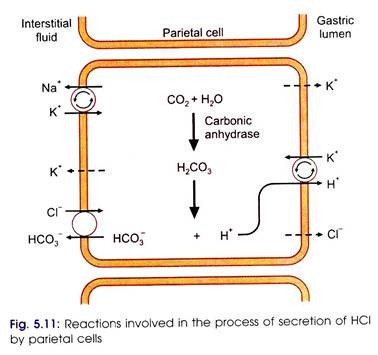
Mechanism of secretion of HCI (Fig. 5.11):
HCI is secreted by the parietal cells. Pure parietal cell secretion has (H+) -150 mEq/liter whereas (H+) of plasma is 0.00004 mEq/liter. It means that the parietal cells have to secrete H+ ions actively. The concentration of H+ ions secreted is directly proportional to the number of parietal cells.
There are two views regarding the source of H+ ions for HCI secretion:
1. Davenport’s view:
According to this, a high energy compound is oxidized to yield H+ ion and an electron. The electron is processed in the mitochondria by the cytochrome system and is accepted by an O2. In the process, OH– is formed and energy is liberated. The H+ ion formed initially uses the energy liberated to form HCI. CI– for this reaction comes from plasma.
2. Modern view:
States that H+ ions in the parietal cells are obtained by active ionization of water yielding H+ and OH– ions OH– should not be allowed to accumulate inside the cell. It is neutralized in the following manner: CO2 produced inside the cell and also contributed from plasma combines with water in presence of carbonic anhydrase (CA) to yield H2CO3. H2CO3 dissociates to yield H+ ion and HCO3– ion. This H+ ion neutralizes the OH– ion. H+ and OH react to form water.
If carbonic anhydrase action is blocked, the entire HCI secretion is inhibited. One of the drugs used to block the action of carbonic anhydrase is acetazolamide (diamox).
The H+ ion formed because of ionization of water is pumped into the intracellular canaliculus in exchange for K+. This H+-K+ pump activity requires the energy supply. ATF is readily available from metabolism of carbohydrates inside the parietal cells to supply the energy required for the activity of the pump.
CI– enters the parietal cell from plasma in two ways:
i. In exchange of HCO3–
ii. By independent diffusion.
Thus it is proved that H+ and CI– are actively secreted into the canaliculus where the coupling occurs to form HCI. The canaliculus is in direct continuation with gastric gland which enters the stomach through the gastric pit.
Immediately following a meal, pepsin and HCI secretion are increased. More H+ ions being utilized, more HCO3–, ions secreted outside. HCO3– will enter blood and hence pH of blood becomes more alkaline. This phenomenon is called post-prandial alkaline tide. Following a meal, kidney excretes more of alkaline urine for short period to maintain the pH of blood.
HCI secretion by parietal cells is stimulated by vagus, gastrin, and histamine (Fig. 5.12). Parietal cells have receptors for the above chemicals. The receptor activity can be selectively inhibited to decrease acid secretion in patients who are secreting excess HCI leading to peptic ulcer formation.
HCI secretion is inhibited by:
a. Acid in the pyloric antrum
b. Acid in the duodenum
c. Fat in the duodenum
d. Hyperosmotic particles in the duodenum
e. Emotional problems, like depression, disappointment
Types of Movements:
1. Receptive relaxation:
As the food fills the stomach, the smooth muscle undergoes relaxation increasing the capacity of the stomach to accommodate the incoming food. This is called receptive relaxation. This is in accordance with LaPlace’s law which states that in a cylindrical structure.
P = T/r
P = Pressure
T = Tension
r = Radius
An increase in the tension should, therefore, cause increase in the pressure. During receptive relaxation, the relaxation of the stomach increases its radius and hence increase in the tension due to stretching of the muscle will not lead to increase in pressure. This facilitates consumption of large quantity of food. The receptive relaxation of gastric smooth muscle is influenced by impulses coming along the vagus nerve.
2. Mixing and propulsive movements:
The conversion of solid food into the fluid chyme and transit of food through the stomach into duodenum is due to gastric peristalsis (a wave of contraction preceded by wave of relaxation). For peristalsis to originate in the stomach, there is slow wave of depolarization starting from the greater curvature.
This is known as gastric slow wave or basal electrical rhythm. It is suggested that upper part of greater curvature acts like a pacemaker for gastric peristalsis. The rate of peristalsis is about 3/min. The contractions are slower in the body of stomach but become stronger and faster in the pyloric antrum (Fig. 5.15). The pyloric orifice leading to duodenum is quite narrow.
The peristaltic contractions of pyloric antrum act like a powerful pump pushing the chyme into pyloric canal. Since the canal is narrow, only a small part of chyme is made to pass through. And the rest of chyme is pushed back (squirting movement) into the cavity of stomach.
This retropulsion helps breaking larger particles into smaller one and also mixing of food with gastric juice. Vagal stimulation increases peristalsis while sympathetic stimulation depresses peristalsis. Therefore, after vagotomy, peristalsis become weaker or abolished.
Gastric emptying time and control:
The normal gastric emptying time for mixed diet is about 2-4 hours. The gastric emptying time depends on the force of peristalsis which is again under the control of factors operating in stomach and duodenum (Fig. 5.16).
Gastric factors:
i. Vagal stimulation increases peristalsis and shortens gastric emptying time. Sympathetic stimulation has opposite effect.
ii. Diet rich in carbohydrate is emptied faster than diet rich in proteins or fats.
iii. Fluids emptied faster than solids.
iv. Quantity of food and gastric emptying time has inverse relationship.
v. Emotional factors: Excitement hastens gastric emptying while grief and sorrow delays it.
Duodenal factors (Fig. 5.16):
Mechanical distension of duodenum, presence of emulsified fats and fatty acids, products of protein digestion, sugars, hyperosmolar substances, HCl, etc., in duodenum delays gastric motility through a reflex known as enterogastric reflex. The reflex is an example for vagovagal reflex.
Even if vagal connection between stomach and duodenum is cut, fats in duodenum can still delay gastric emptying. It is brought about by hormonal factor and the hormones involved secretin and CCK-PZ (cholecystokinin pancreozymin), GIP, etc. Duodenum has got specific receptors for HCl, fats, osmolar substances, etc.
Significance of duodenal inhibition of gastric motility:
1. Small amount of chyme is presented to small intestine for better digestion and absorption.
2. Acidity of the chyme needs to be neutralized by alkaline pancreatic juice and bile. Some time is needed for these juices neutralize hydrogen ions.
Contractions of empty stomach:
Empty stomach is capable of contractions called hunger contractions or hunger pangs. Hunger pangs appear, if fasting is there for more than 12 hours. Hunger pangs disappear once food is taken in. Impulses from hypothalamus and the vagus are responsible for initiating these contractions.