The following points highlight the eight types of Anterior Pituitary Gland. The types are: 1. STH (Somatotrophic Hormone) 2. Prolactin or LTH / PRL 3. Adrenocorticotropic Hormone (ACTH) 4. Thyroid Stimulating Hormone (TSH) 5. FSH 6. LH/ICSH 7. MSH (Melanocyte Stimulating Hormone) 8. Oxytocin and Vasopressin.
Contents
- Anterior Pituitary Hormone: Type # 1. STH (Somatotrophic Hormone):
- Anterior Pituitary Hormone: Type # 2. Prolactin or LTH / PRL:
- Anterior Pituitary Hormone: Type # 3. Adrenocorticotropic Hormone (ACTH):
- Anterior Pituitary Hormone: Type # 4. Thyroid Stimulating Hormone (TSH):
- Anterior Pituitary Hormone: Type # 5. FSH:
- Anterior Pituitary Hormone: Type # 6. LH/ICSH:
- Anterior Pituitary Hormone: Type # 7. MSH (Melanocyte Stimulating Hormone):
- Anterior Pituitary Hormone: Type # 8. Oxytocin and Vasopressin:
Anterior Pituitary Hormone: Type # 1. STH (Somatotrophic Hormone):
STH is secreted from STH-cells of adenohypophysis. It is a peptide hormone. Its molecular weight is about 22 KD in all mammalian species. It is made up of 191 amino acid residues. It consists of 2 disulfide bridges (-S-S-) between adjacent cysteine residues at 53 and 165, 182 and 188.
The N-terminal and c-terminal residues are both phenylalanine (Phe). After synthesis, the hormone is stored in Golgi apparatus. It has small c-terminal loop and large central loop (Fig. 5.1).
This hormone promotes DNA, RNA and protein synthesis via insulin like growth factor (IGF-1) in liver, chondrocytes, muscles and somatic cells.
It follows following functions:
1. General Body Growth:
It stimulates growth rate of all growing cells by increasing cellular mitosis and synthesis of cellular material.
2. Skeletal Growth:
It controls growth of bones, especially the formation of epiphyseal cartilage, in association with protein factor somatomedin (mol. wt. 7000 Dt).
3. Protein Metabolism:
This hormone enhances the uptake of amino acids. It also promotes synthesis of proteins in different tissues like muscles and other cells. It stimulates nitrogen retention and positive nitrogen balance.
4. Carbohydrate Metabolism:
It reduces glycolysis and elevates blood sugar level by enhancing the release of glucose from the liver due to glycogenolysis. Hence it shows diabetogenic effect or anti insulin effect. It inhibits insulin secretion from p-cells of pancreatic islets.
5. Lipid Metabolism:
It shows lipolytic effect. It causes loss of body fat which is mobilized from adipose tissue. It increases the free fatty acid level in plasma, lipid level in hepatic cells, P-oxidation and ketosis in liver.
6. Growth of Mammary Gland:
It may help in growth of mammary gland and also stimulates lactation.
7. Mineral metabolism:
It increases the intestinal absorption of Ca++. This hormone shows anabolic effects on Mg++, K+ and Na+ metabolism.
Anterior Pituitary Hormone: Type # 2. Prolactin or LTH / PRL:
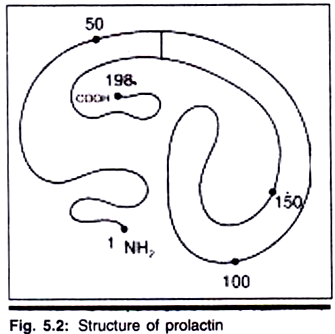
This hormone is secreted from LTH-cells of adenohypophysis. Prolactin is protein hormone. Its molecular weight is about 23 KD. It is made up of 198 amino acid residues. It has 3 disulfide bonds between cysteine residues at 4 and 11, 58 and 73 and 190 and 198. It has a small N-terminal loop and c-terminal loop; whereas central loop is large. This hormone is stored in Golgi apparatus (Fig. 5.2).
Prolactin follows following functions:
1. Mammotropic Action:
This hormone stimulates the proliferation of mammary glands during pregnancy.
2. Milk Secretion:
It is responsible for lactation in mammals after giving birth.
3. Luteotropic Action:
It helps in maintenance and secretion of corpus luteum in mouse, rat, ferret and possible synergism in other species of mammals.
4. Carbohydrate Metabolism:
It helps in glycogenolysis and produce hyperglycemia.
5. Lipid Metabolism:
It promotes deposition of fat in adipose tissue.
6. RNA Synthesis:
It helps in synthesis of RNA and RNA polymerase.
7. On Growth:
It helps in growth of sebaceous gland tissue, maturation of hair, growth of erythrocytes etc.
8. Anti-gonadotropic Action:
This hormone decreases the steroidogenic actions of gonadotropins and also inhibits GnRH secretion of hypothalamus.
Anterior Pituitary Hormone: Type # 3. Adrenocorticotropic Hormone (ACTH):
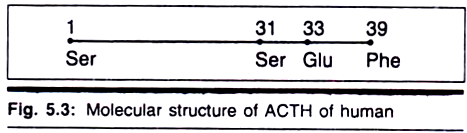
ACTH on corticotropin is secreted from ACTH cells of adenohypophysis. It is a small peptide hormone. It is made up of single chain polypeptide consisting of 39 amino acid residues. Serine and phenylalanine present at N-terminal and c-terminal ends respectively (Fig. 5.3).
The first 24 N-terminal (1-24) amino acid residues of ACTH are essential for its full activity. The most potent segment of activity is from residue 15-18. The species variations are confined to the amino acids that occupy 31 and 33 position. Its molecular weight is about 4.5 KD.
ACTH shows following functions:
1. It has a stimulatory effect on the hormone producing capacity of the adrenal cortex.
2. It accelerates gluconeogenesis.
3. It has intrinsic melanocyte stimulating activity.
4. It helps in transfer of cholesterol from plasma to fasciculata cells.
5. It enhances adipose tissue lipolysis to increase the mobilization of fatty acids from the adipose tissue into the blood (adipokinetic effect).
6. It may act directly on adipocytes to activate adenyl cyclase and increase cAMP.
7. It stimulates Cytochrome P450 and other enzymes.
8. It promotes binding of cholesterol to the mitochondrial cytochrome P450 in fasciculata cells for hydroxylation of cholesterol.
Anterior Pituitary Hormone: Type # 4. Thyroid Stimulating Hormone (TSH):
This hormone is secreted from TSH cells of adenohypophysis. It is a glycoprotein hormone. Its molecular weight is about 30 KD. This hormone consists of two subunits α and β joined by non-covalent bonding. The α subunit consists of a polypeptide of 92 residues in human and 96 residues in other mammalian species. The a-subunit binds with two oligosaccharide chains joined to its specific Asparagine’s (Asn) residue by N-glycosidic bonds. The amino acid sequence is similar in different mammalian species.
The specific biologic activity is determined by the p-subunit. The β-subunits exhibit different amino acid sequences in different species. The β-subunits are composed of 112-118 amino acid residues. Each subunit possesses 12cys residues. The two subunits have several inter-chain – S-S- linkages. The constituent sugars are D- mannose, D-galactose, L-fucose, N-acetyl neuraminic acid, D-glucosamine and N- acetylated D-galactosamine.
TSH follows the following functions:
1. It controls the growth and activity of thyroid gland.
2. It stimulates the synthesis and secretion stored thyroid hormones from the thyroid follicle.
3. It increases the nucleic acid content, transcription, translation, mitotic figures and cell sizes in the thyroid gland.
Anterior Pituitary Hormone: Type # 5. FSH:
The hormone FSH is secreted from FSH cells of adenohypophysis. It is chemically made up of glycoprotein. Its molecular weight is about 34 KD. This hormone also consists of 2 subunits α and β. The p-subunit consists of 118 amino acid residues; otherwise the structure is same like TSH.
This hormone shows following functions:
1. In male, it helps to increase the size of seminiferous tubules and growth of spermatogenic cells. It also stimulates testicular Sertoli cells to synthesize specific androgen binding protein (ABP) which carry testosterone from leydig cells to the seminiferous spermatogenic cells.
2. In females, it stimulates the growth of immature ovarian follicles to graafian follicles and prepares them for ovulation. It also stimulates ovarian follicular cells to synthesize and release a serine protease, plasminogen-activator, which initiates ovulation.
3. It may help in growth of gonads.
4. It up-regulates the number of LH receptors on ovarian granulosa cells to enhance their sensitivity to LH.
Anterior Pituitary Hormone: Type # 6. LH/ICSH:
LH/ICSH is a glycoprotein hormone. Its molecular weight is about 29 KD. In female, it is called as LH, where as in male it is known as ICSH. In both case, molecular configuration is same. The structure of LH/ICSH is same like TSH. Only the p-subunit is constituted by 112 amino acid residues.
The functions of LH/ICSH are given below:
1. Actions of LH:
(a) It helps in complete development of graafian follicle and induces ovulation.
(b) After ovulation, LH causes proliferation of granulosa cells and changed the ruptured follicle into corpus luteum.
(c) It stimulates steroid genesis in luteal cells to secrete hormone progesterone.
(d) It stimulates granulosa cells to secrete plasminogen activation.
(e) Prolonged LH action down regulates LH receptors, lowering their number on corpus luteum cells by enhancing their endocytosis and degradation. This lowers the LH sensitivity of the luteal cells and decreases their steroidogenic response to LH.
(f) It helps in growth of secondary sex characters in females.
2. Actions of ICSH:
(a) It stimulates the development and functional activity of leydig cells or interstitial cells of testis.
(b) It stimulates the leydig cells for secretion of testosterone.
(c) Indirectly promotes spermatogenesis by synthesizing testosterone.
(d) It helps in the development of secondary sex characters in males.
Anterior Pituitary Hormone: Type # 7. MSH (Melanocyte Stimulating Hormone):
MSH is secreted from pars inter-media of pituitary gland. It is also known as intermedin. In mammals, the type of MSH is isolated α-MSH and β-MSH. Both types are simple’ linear polypeptide chain-α-MSH is found in pituitaries of all mammals. α-MSH contains 13 amino acid residues where N- terminal serine in acetylated and the C-terminal valine is in the amide form.
Thus, in a-type, the terminal groups are blocked. The β-MSH of all mammalian species contain 18 amino acid residues, except human beings, where additional 4 amino acid residues are found at the N-terminal end, thus it becomes longer (22 amino acids).
Furthermore, in humans, α-MSH is lacking. In human, pars inter-media is highly reduced. Pregnancy is the only physiological state in which MSH is detectable in plasma, the source of which may be placenta or pregnancy—induced pituitary intermediate lobe.
The function of MSH is given below:
1. MSH helps in synthesis of melanin in melanocytes and help in darkening of skin, especially in tropical countries to protect the skin from solar UV rays.
2. It helps in alteration in the amount of pigmentation on colour change. For instance, in polar hare, dark brown summer pelage to a white winter coat. It is also found in Siberian hamster. This change of colour in different season is a protective phenomenon.
3. This hormone is known to affect CNS in human and laboratory mammals. These effects include arousal, increased motivation, memory retention, increased learning ability.
4. Clinically, it is observed that administration of supernatant analog of α-MSH may cause erection of penis.
Anterior Pituitary Hormone: Type # 8. Oxytocin and Vasopressin:
Oxytocin and vasopressin are two neurohypophysial hormones. In the early 1950, two posterior pituitary hormones oxytocin and vasopressin were identified determined their individual activities. Du Vigneud et al. (1953) determined the chemical nature of oxytocin and vassopressin. Acher and Chavet (1953) identified the amino acid sequence of vasopressin. In the same year, Tuppy (1953) identified the amino acid sequence of oxytocin.
Oxytocin and vasopressin are found within the pars nervosa of most mammalian species. These two hormones are localized within the axonal endings. Each hormone is transported through axons in association with specific carrier protein, called neurophysins. There are two specific neurophysins for oxytocin. Oxyphysin is the neurophysin, whereas pressophysin in case of vasopressin.
Each hormone is a non-apeptide amine, containing cysteine molecules at position 1 and 6 linked by disulfide bond (-S-S-). Both oxytocin and vasopressin as structurally similar except that isoleucine (lie) is replaced by phenylalanine (Phe) and Leucine (Leu) by arginine (Arg) at 3 and 8 position (Fig. 5.4).
Vasopressin obtained from pigs and marsupials differ from other mammals includin human, where Arg is replaced by Lysine (Lys) at position 8. Thus vasopressin can be designated as Arginine vasopressin and Lysine vasopressin. In mammals, vasopressin is also called as AVP.
Actions of Oxytocin:
1. Lactation:
In mammals, role of oxytocin in lactation is the characteristic feature. During suckling of baby, neural impulses from nipple go to neurohypophysis and stimulate the neurohypophysial cells for secretion of oxytocin. Oxytocin then stimulates myoepithelial cells of mammary gland for secretion of milk.
2. Uterine effect:
During parturition, it stimulates the contraction of uterine smooth muscles, thus facilitating child birth.
3. The reflex release of oxytocin during coitus results in the contraction of uterine muscles with a consequent aspiration of semen into the uterus. It also helps in the movement of sperm in the uterus.
4. It produces hyperglycemia.
5. Helps in water and Na+ metabolism.
6. It lowers the blood pressure and slightly dilates the coronary vessels.
7. It helps in contraction of gall bladder, intestine and urinary bladder.
8. Plasma oxytocin increases during sexual arousal in both men and women.
9. It may control the feeding behaviour.
Actions of Vasopressin:
1. Antidiuretic action:
Vasopressin primarily increases the permeability of renal tubules, so reabsorption takes place and urine volume becomes reduced. Hence this hormone is also known as ADH (anti diuretic hormone).
2. Vasoconstriction:
It stimulates the contraction vascular smooth muscles to bring about peripheral arteriolar vasoconstriction. During hemorrhage, to much vasopressin liberate and help to contract the blood vessel check the blood flow.
3. It constricts the coronary arteries and raises the blood pressure.
4. It reduces the heartbeat.
5. It stimulates the contraction of muscular walls of ureter and urinary bladder.
6. Helps in sugar metabolism and shows glycosouria, glycogenesis and hyperglycemia.
7. It decreases the rate of perspiration.