Here is a compilation of essays on the ‘Process of Fertilization in Animals’ for class 9, 10, 11 and 12. Find paragraphs, long and short essays on the ‘Process of Fertilization in Animals’ especially written for school and college students.
Contents
Process of Fertilization in Animals
Essay Contents:
- Essay on the Introduction to the Process of Fertilization in Animals
- Essay on In Vivo Fertilization in Animals
- Essay on In Vitro Fertilization in Animals
- Essay on Post Fertilization Events in Animals
Essay # 1. Introduction to the Process of Fertilization in Animals:
Fertilization is a complex process which involves the fusion of male and female gametes followed by the fusion of their cytoplasm. Fertilization begins with the sperm’s approach to the egg and ends with the fusion of egg and sperm pronuclei. It involves a series of events.
The process of fertilization has dual independent functions:
(i) To cause the egg to start developing i.e. Activation, and
(ii) To inject a male haploid nucleus into the egg cytoplasm, i.e. Amphimixis.
Activation Involves:
(i) The completion of second maturation division, if not occurred earlier;
(ii) The egg cortex to form fertilization membrane outside the plasma membrane;
(iii) The egg cytoplasm to start various metabolic reactions; and
(iv) Stimulation of mitosis for cleavage by contribution of sperm’s centriole to the egg.
Amphimixis is the most important event occurring in the life of all animals and plants and involves:
(i) The intermingling of paternal and maternal hereditary characters in the offspring;
(ii) Restores the diploid state of animal cell; and
(iii) Includes genetic variations in the species. The genetic variations provide the raw materials to the natural selection for speciation (species formation).
The process of fertilization has been studied mostly in marine invertebrates, such as, sea urchins, polychaetes, echinroids etc. whose eggs are typically translucent and without much yolk. Among vertebrates most fertilization studies have been done in amphibians and mammals.
Attention has been focussed on amphibians because they are available and suitable for analytical and experimental procedures, and on mammals because man himself is a mammal and the need to know what happens is great.
Essay # 2. In Vivo Fertilization
in Animals:
In most animals the act of fertilization requires the following fundamental conditions for its fulfilment:
(1) In most animals fertilization requires a fluid medium which may be sea water in marine forms, fresh water in fresh water forms or some body fluid in viviparous animals.
(2) The life span of gametes is limited. Mature eggs quickly “over ripe”, they must be activated promptly if they are to be activated at all eggs that are shed into the water like those of most invertebrates, fish and amphibians have shorter life span while those fertilized within the body of the female generally have a longer life span; for example, the human egg can be fertilized for atleast 24 hours after ovulation.
Sperms are also short lived, but there are many exceptions to this rule in nature. For example, in bat viable sperms may persist in the female reproductive tract for many months in the winter, during hibernation. Further, life span of human sperm in female genital tract is 24 hours.
(3) To increase the probability of fertilization, the number of sperms must exceed the number of eggs. In mammals a single ejaculation may range from 0.05 ml in bat, 2 ml in rat, 3 ml in man to 500 ml in boar containing 6 million, 2 to 5 million, 1 million cells per microlite respectively.
Post-Fertilization Changes in the Egg Cytoplasm:
The penetration of spermatozoa into the egg causes far-reaching displacements of the cytoplasmic constituents. As a result, the distribution of various cytoplasmic substances and inclusions in a fertilized egg may be very considerably different from that in the unfertilized egg and even quantitatively new areas may appear.
As a result of the extrusion of cortical granules, a large part of the original outer egg cell surface is replaced by the inner surface which surrounds the cortical granules and now are averted on the exterior. Most spectacular post-fertilization displacements in the egg cytoplasm have been observed in ascidian, Styela partita and in frog. In both these animals, there establishes a bilateral symmetry in the cytoplasm of fertilized eggs.
Displacements of cytoplasmic substances in the egg of asicidian Styela partita are as under:
The mature egg is covered by a layer of cortical cytoplasm containing yellow granules. The moment spermatozoon enters the egg near the vegetal pole, the yellow cortical cytoplasm falls into violent commotion.
The yellow cytoplasm begins to stream down along the surface of the egg toward vegetal pole, and accumulated as a cap. As the male pronucleus penetrates deeper into the cytoplasm and moves toward female pronucleus, the yellow cytoplasm, reverses its movements and streams upward only on the side where the spermatozoon entered the egg.
Just before the first cleavage, the yellow cytoplasm forms a cresentic area (mesodermal crescent) just below the equator of the egg. Simultaneously, a crescent of light gray cytoplasm (notochordal crescent) appears sub-equatorially on the opposite side of the egg.
Thus, in a fertilized egg, four different kinds of cytoplasmic regions are now present:
(i) The yellow cytoplasm on one side, and
(ii) The light cytoplasm on the other side. These two together form a belt surrounding the egg just below the equator. Below this zone toward the vegetal pole,
(iii) The cytoplasm in slaty grey colour contains abundant yolk granules and in the subcortical layer, there are a large number of mitochondria. But the cytoplasm in
(iv) The animal hemisphere contains less yolk and a few mitochondria and appears more transparent. Thus, the cytoplasmic displacements following fertilization not only bring some kind of cytoplasm to more restricted areas, but also give the egg a distinct bilateral structure.
Monospermic and Polyspermic Fertilization:
Monospermic:
When only one spermatozoon penetrates into the egg to fertilize it, the type is called monospermic fertilization, as in most classes of animal kingdom (e.g. coelenterates, echinoderms, bony-fishes, frog and mammals.)
Polyspermic:
It is of two types:
(a) Pathological Polyspermy:
This type occurs in pathological conditions when many spermatozoa penetrate the ova of a normally monospermic animal.
(b) Physiological Polyspermy:
When many spermatozoa penetrate ova as a whole, such kind of fertilization is called polyspermic fertilization. This type of fertilization occurs in animals having yolky eggs like molluscs, selachians, urodeles, reptiles and birds.
In such eggs only one spermatozoon participates fully in the development of the embryo, the rest degenerate sooner or later. This type of polyspermy, because it has some physiological significance, is called physiological polyspermy.
Significance of Fertilization:
The process of fertilization has following significances:
(1) The fertilization ensures the usual specific diploidy of the organisms by the fusion of the male and female pronuclei.
(2) It introduces genetic variations in the species.
(3) It activates the egg to start cleavage.
Essay # 3. In Vitro Fertilization in Animals:
Fertilization is the process of fusion of male and female gametes.
It can be differentiated on the basis of its site of occurrence into two main types:
(i) Natural fertilization, and
(ii) Artificial (in vitro) fertilization.
Natural fertilization occurs as a most common process either within the female genital tract or outside the body of the parents. However artificial fertilization always occurs outside the body of the animals in test tubes.
During the last few decades, great effort has been directed in refining in vitro fertilization and embryo transfer technology, and sufficient progress in this direction has actually been made not only in animals but also in human beings. It is hoped that these techniques will lead to genetic improvement of farm animals leading to high growth rates and increased yield of their products such as milk.
In human beings after successful recovery of viable oocyte (secondary oocyte), in vitro fertilization and embryo transfer, followed by normal development of the fetus, the birth of a baby on July 25, 1978, named Loise Joy Brown is considered to be a sensational event of great scientific importance and human health care.
This technique is being widely used in many countries to provide the pleasure of having their own babies to couples suffering from infertility. Infertility can be due to any one of a variety of reasons in male or female or both.
Infertility in Female:
i. Tubal Infertility:
This type of infertility occurs due to damage or non-functional fallopian tubes, which receive oocytes from the follicles of ovary and provide space for fertilization. Some of the approaches to cure tubal infertility include transplantation or replacement of the tubes by grafting from a healthy individual. In vitro fertilization technique is gradually replacing this approach of surgery.
In this case the ovaries do not function normally and produce ova due to structural deformity, diseases, or incomplete development of the ovaries.
In this type, the uterus is not capable of receiving the embryo due to structural defects or hormonal disorders.
In this case no valid explanation can be given for the cause of infertility. It may be due to failure of fertilization or abnormal fertilization.
Infertility in Male:
For normal fertility the number of spermatozoa required in human semen is 15 to 20 million per milliliter. Reduced number of sperms in a male is often described as oligospermia while presence of very few sperms or their total absence is known as azoospermia. Male infertility may be due to sterile sperms (non-motile), non-functional or damaged epidydymis and non-functional accessory glands.
Assessment of Patients:
The female partner included for in vitro fertilization should fulfill the following conditions:
(a) She should be physically fit and healthy to carry the resultant pregnancy so that surgical procedure if involved in vitro fertilization and embryo transfer will not create any problem.
(b) Her ovaries should be accessible for oocyte recovery.
(c) Her uterus should be capable of accepting and sustaining pregnancy for full term of nine months.
Male partner is examined for only an appropriate concentration of motile sperms.
Different steps involved in in vitro fertilization include:
(i) Collection of motile sperms,
(ii) Collection of oocytes,
(iii) In vitro fertilization of the oocyte, and
(iv) Embryo transfer – Implantation of the resulting zygote in the uterus of the female.
Treatment of the Patient for In Vitro Fertilization:
The female patients for in vitro fertilization are required to record the commencement of each of their menstrual cycle for at least six months so that decision may be taken for:
(1) Admitting the patient to the hospital,
(2) Date of urine sampling for Leutenizing hormone surge,
(3) Date of administration of Human Chorionic Gonadotropin to control the final stage of follicular development.
Nature of Cycle for Follicular Development:
The nature of treatment prescribed for female partner of the couple will depend upon which of the following three cycles is utilized for oocyte recovery for in vitro fertilization:
(1) In the natural cycle spontaneous LH surge is detected by urine or plasma sampling at 3 to 6 hours intervals. A spontaneous cycle has the advantage of early term pregnancy and natural hormonal environment for embryo transfer. The disadvantage includes the availability and recovery of only one oocyte leading to low success rate of in vitro fertilization and embryo transfer.
(2) In the stimulated cycle multiple development of follicles is stimulated by Clomiphene or HMG but LH surge is spontaneous and detected as above. HCG is also administered to check inhibition of LH surge caused by HMG.
The advantage of stimulated cycle is the availability of multiple follicles and oocytes so that several embryos are available for embryo transfer. The disadvantages are the recovery of oocytes at different developmental stages and abnormal environment for embryo transfer, which cause increased risk of abnormal pregnancy.
(3) In controlled cycle the development of follicles is arrested at the optimum stage of maturation by the administration of HCG. The advantage of this cycle is that the oocyte recovery can be performed through laparoscopy at a time convenient to the doctor and the patient.
Ovarian Stimulation:
Once the decision has been taken that the stimulatory cycle needs to be used, the patients need to be given dose of Clomiphine and HMG. Clomiphine is given at the optimum rate of 150 mg per day from fifth day to ninth day of the cycle.
Some patients do not respond to five- day course so that prolonged administration for 10 days may be required. This prolonged treatment causes the antioestrogen effect so that uterus receptivity for implantation of embryo may be reduced leading to abortion.
However, the abortion rate is low if HMG is used instead of Clomiphine but HMG is costly and a combination of Clomiphene and HMG is often used.
Monitoring Ovarian Stimulation:
The following parameters are used as indicators for ovarian stimulation to help collection of oocytes at optimum stage of development:
(1) Prediction of the day of LH surge on the basis of data on length and dates of menstrual cycles.
(2) Temperature chart showing the rise in temperature at pre-ovulatory and post-ovulatory stages.
(3) Changes in cervical mucus score indicate follicular development; it begins to rise five days before LH surge reaches a maximum level a day before and falls sharply on the day of LH surge.
(4) Plasma or urinary estrogen levels which can be estimated at 24 hour urine collection and are used for timing the LH surge and HCG injection.
(5) Ultrasonic determination of follicular size.
(6) Detection of LH surge and progesterone determination.
Spontaneous LH Surge:
For accurate prediction of ovulation time, LH peak is most useful. LH can re assayed in urine either by haemagglutination or by radioimmunoassay to allow correct prediction of time for laparoscopy.
Administration of HCG for Controlled Ovulation:
HCG is administered so that ovulation is controlled.
The decision to administer HCG is made on the basis of:
1) The day of the menstrual cycle,
2) Size and number of follicles estimated through ultrasonic examination. Size of follicle should be at least 1.9 cm in diameter. HCG is administered before LH surge.
Recovery of Oocytes:
Several methods for oocyte recovery were used in the past.
They Include:
(1) The follicle is totally aspirated and oocyte identified in the follicular aspirate. If an oocyte is identified in the aspirate, further aspiration is not necessary.
(2) The excised ovary is minced for oocyte recovery.
(3) Intact follicles are dissected prior to puncture to study developmental stages.
(4) Follicles are dissected under the microscope and oocytes are recovered.
Equipment and Techniques for Laparoscopy:
Recovery of oocytes is the most convenient and efficient by laparoscopic equipment. It permits the visualization of ovary through a monitor, and aspiration of the follicular fluid containing the oocyte.
In this technique, the necessary surgical manipulation of ovary sensors, laparoscopic scissors and an aspirating apparatus are inserted into the abdomen of the female through a suitable tube. This procedure involves minimum surgical intervention and causes very little damage to the ovary, and is quite convenient.
Ovulating follicles are selected for aspiration. Follicles that may have ova capable of undergoing fertilization are smaller than 1.5 cm. The suction apparatus should be tested using culture medium to avoid spillage of fluid and loss of oocyte due to failure of the pump.
The follicular fluid aspirated completely from ovulating follicles is 4 – 12 ml in volume. It is straw colored although it sometimes is contaminated with blood. As soon as blood appears in the aspirating tube, heparinized culture medium should be added to the aspirate to avoid clotting because if blood clot appears in aspirate, the ovum may not be easily identified, isolated and fertilized.
As the fluid is aspirated, walls of the follicles collapse. The aspirate may be examined and oocyte identified, failing which repeated flushing of the follicular fluid with heparinized culture medium is performed to get the oocyte through respiration of distended follicle.
This may be repeated as often as necessary until the oocyte is recovered. For recovery of the fully mature oocyte, follicular monitoring and timing between LH and HCG administration should be carefully interpreted since one would like to culture the oocyte in vitro for a minimum period before fertilization. This will increase the chance of fertilization and subsequent embryo development.
Oocyte Culture and in Vitro Fertilization:
Naked oocyte is identified under the microscope and is handled with great care. The oocytes are incubated for 5-10 hours after oocyte recovery depending upon the estimated maturity of the follicles and oocytes.
The following four culture media have been used for oocyte culture and in vitro fertilization:
(1) Modified Ham’s F10 medium.
(2) Earl’s solution.
(3) Modified Whitten’s culture medium.
(4) Whittingham’s Tc medium.
The culture medium is prepared weekly and tested by culturing mouse embryos from 2- cell stage to blastocyst stage. The use of the same medium for fertilization and embryo culture has actually simplified the fertilization and culture techniques of embryo.
Techniques of Semen Preparation:
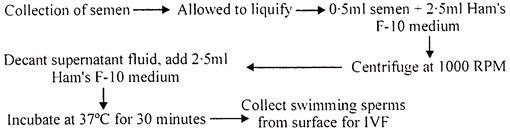
Semen is collected at site by masturbation 60 – 90 minutes before insemination. Semen is mixed with Ham’s F-10 medium in proportion of 1 : 5, centrifuged at 1000 RPM for 5 minutes. The supernatant fluid is decanted off and the sperm pellet at bottom of the tube is mixed with culture medium and incubated at 37°C for 30 to 45 minutes when actively motile spermatozoa swim up at the top of the tube forming a cloud. The percentage of motility in the final preparation is 90%. A sample is taken from the surface because it contains the most active spermatozoa.
A sample containing 10,000 – 50, 000 motile spermatozoa is added to 10 µl – 1ml of culture medium containing the oocytes. After insemination oocyte is left for 12 – 13 hr and then examined in a petri dish containing culture medium. The oocyte should contain two pronuclei and two polar bodies. Any abnormality like presence of multiple pronuclei, granulation of cytoplasm or abnormal shape is noted and such embryos are not used for transfer.
First cleavage occurs 24 – 30 hr after insemination and each subsequent division should occur with in 10 – 12 hours thereafter. If cleavage does not occur with in 24 hours, this suggests abnormal oocyte, which should not be used for embryo transfer.
Success has been achieved from the transfer of 1 – 16 celled embryos to the uterus. Embryo in vivo stays in Fallopian tube up to 8 – 16 celled stage and then move to wards uterus. Prolonged culture of an embryo in vitro reduces viability and thus reduces the pregnancy success rate.
The best stage is perhaps 2-4 cells, although these early embryos may not survive in uterus. Multiple embryos may also be transferred to increase the chance of subsequent pregnancy, which the patient may not like because this may lead to multiple pregnancy.
Techniques of Embryo Transfer:
The patient is given 10 mg of diazepam (Valium) orally before embryo transfer. Embryo transfer is negotiated through cervical canal.
Following Steps are involved in Embryo Transfer:
(1) A sterile bivalve vaginal speculum is gently inserted to visualize the cervix.
(2) When cervix is exposed and ready for transfer, embryo is drawn into a teflon catheter having 10 ml of tissue culture medium. Teflon is used due to its low adhesiveness. It reduces the chance of carrying cervical secretions into the uterine cavity.
(3) The teflon catheter is then passed down an outer teflon sheath which protects the inner catheter from vaginal contamination.
(4) The catheter is then inserted into the uterine cavity just short of fundus, using the information about the distance from the fundus to external cervical orifice.
(5) Embryo is gently injected in culture medium and the catheter and canula are gently withdrawn.
(6) Catheter is examined under the microscope to ensure that the embryo has been expelled.
The above steps should be performed with greatest care since incorrect placement of embryo or the use of excessive quantity of fluid for transfer may lead to the expulsion of the embryo from the uterine lumen. After transfer of the embryo, the patient is advised to rest for 2 – 7 hours and to abstain from intercourse for atleast a week. No hormonal support is advised after embryo transfer.
Application of In Vitro Fertilization and Embryo Transfer:
The in vitro fertilization and embryo transfer technologies offer several advantages, which are manifest in their varied applications.
These are as follows:
(1) These technologies achieve a surprisingly rapid rate of multiplication of animals of selected superior genotype. In natural course, a single female will produce a single progeny in about one year but using superovulation and embryo transfer technology, it is feasible to collect around 36 embryos from one female in one year.
A single female can be induced to ovulate on an average, 6 times a year, and in each ovulation cycle, about six healthy transplantable embryos are obtained. Assuming an average success rate of 50% in embryo transfer, an average of 18 progeny can be derived from one superior female in one year.
(2) Each embryo can be split into two to four parts, each of which would develop into a separate progeny; this is called embryo splitting. By combining embryo splitting with superovulation and embryo transfer technique, the rate of multiplication can be further increased.
(3) Young embryo can be frozen and stored in liquid nitrogen for up to ten years or more and used at a subsequent date. The frozen embryos are far easier to transport and present negligible quarantine problems as compared to the animals themselves.
Freezing and storage of young embryos in liquid nitrogen at -196° C is known as cryopreservation. The embryos are first treated with a suitable concentration of a compound like glycerol, which protects them from injury during freezing, and thawing; such compounds are called cryoprotectants. They are then cooled at a slow rate to -38° C, ordinarily employing a programmable controlled rate freezer.
These embryos are then plunged into liquid nitrogen and stored at -196° C. The embryos are thawed at a very rapid rate by immersing the ampoule carrying them into a water bath maintained at 0°C.
(4) Superior genotype that is unfit to carry the fetus to full term can serve as donors of the young embryos.
Disadvantages:
(1) A high degree of expertise is required for an efficient and successful operation.
(2) The cost of producing each progeny is several folds higher than that from natural events.
(3) The donor females are removed from production for the period they are used as donors of young embryos.
Essay # 4. Post Fertilization Events
in Animals:
In eutherian mammals the fertilization in internal in the oviduct and the fertilized eggs are retained in the maternal uterus (viviparous development). The developing embryo of such a viviparous animal establishes a direct contact with the uterine wall as a graft that grows and develops into placenta. In birds and reptiles, placenta serves for waste storage and for respiratory exchange but in mammals it serves as a selective organ for all metabolic exchange between mother and the embryo.
Because of accepting shelter into the maternal body (implantation in the uterus) the embryo is almost at the mercy of the mother and perishes swifty if her hormonal, physiological and immunological adaptations to pregnancy are inadequate.
All the mammals except prototherian mammals which are oviparous (e.g. Omithorynchus) or ovoviviparous (a condition of egg laying mammals in which the eggs though develop inside the maternal body but are not supplied with maternal nourishment e.g. Echidna) are viviparous.
The viviparity is an adaptation to adverse climatic conditions. Birds have not developed viviparity because of burden of carrying the unborn young in flight. However, bats which are mammals carry their offsprings in flight.
In all mammals the sexes are separate, sexual dimorphism is well marked and the reproductive physiology of both sexes has close resemblance.
Organisation of Gametes:
The Spermatozoon:
The fully developed sperm has a head, a neck, a middle piece and a tail. The entire sperm is a single cell with the nucleus occupying a greater part of the head.
Structure of Head:
The sperm head enhibits a diversity of shape in different groups. The head of human sperm is a pear shaped structure with the narrow part of the pear directed anteriority. The head is nearly 0.004 mm to 0.005 mm long and its thickness is about 0.003 mm. Its anterior tip is differentiated as acrosome, which is a complex, vesicular structure originating from the Golgi apparatus during the formation of the sperm.
Acrosome enables the sperm to penetrate through the egg membranes and to establish connection with the egg cytoplasm. Externally the head is covered by a cell membrane. The acrosome remains in between the cell membrane and the narrow part of the nucleus (Fig. 11).
Structure of Neck:
Neck joins the head to the middle piece. It is very short and cylindrical. The cell membrane of the head is continuous over the neck with the cell membrane of the rest of the sperm. A centriole is situated at its anterior end which is composed of 27 microtubules arranged in nine groups of three tubules each. The central part of the neck contains the anterior end of the axial filament. One or two mitochondria may be present in the neck.
Middle Piece:
It is a rod like portion of the sperm behind the neck and is about 6 µm (0.006 mm) long and 1 µm (0.001 mm) thick. Its central core is occupied by the axial filament. Surrounding the axial filament there are many mitochondria which are arranged end to end to form a spiral.
Tail:
It is a filamentous structure about 0.055 mm long. Along the centre of the tail runs the axial filament. It is also known as principal piece. Maturation of sperms takes place in the epididymis. The sperms produced in the testies enter the epididymis and remain there for sometime.
It is believed that some changes takes place in the sperm here. The sperm become motile. A human sperm can penetrate an ovum only when it remains for some time in the fallopian tube of the female. Development of this ability is called capacitation of the sperm.
The Ovum:
The human ovum when released from the ovary is 100 to 150 µm in diameter. The ovum apparently does not possess any true vitelline membrane. Immediately surrounding the cell membrane, there is a thick transparent, perforated non-cellular layer, the zona pellucida. Surrounding the zone pellucida is a layer of follicle cells derived from the ovary.
This layer of cells is called the corona radiata. The actual ovum or the secondary oocyte has a cell membrane or oolemma. A distinct round nucleus is the ovum is formed only after the second polar body is thrown out of the time; of fertilization. The human egg possess very little yolk hence called microlecithal egg (Fig. 12).
In the ovary the ovum remains surrounded by several layers of follicle cells (corona radiata cells) which in turn remain surrounded by a fluid, the liquor folliculi. Outside the fluid there are again several layers of follicle cells (granulosa cells). Outside the granulosa cells there is a theca composed of cells and connective tissue fibres.
This structure is known as Graffian follicle. It is a spherical structure. Graffian follicle is a mature follicle and at any time there is one Graafian follicle in the ovary where as immature follicles are many. All these follicles are embedded in a mass of connective tissue, blood vessels etc.
The entire ovary is surrounded by an extremely thin epithelium. The germinal epithelium and a thin layer of connective tissue called tunica albuginea. A Graffian follicle is situated just under these layers. Normally, every 14th day one ovum is released from an ovary after the onset of maturation and an ovum is probably released alternately from each ovary.
When a Graffian follicle fully matures, the ovum with its zona pellucida and corona radiata cells gets separated from the granulosa cells and floats in the liquor folliculi. A part of the germinal epithelium, theca and granulosa cells surrounding the ovum get thinner and thinner at one place and ultimately break releasing the liquor folliculi and ovum with its corona radiata cells into the fimbriated end of the fallopian tube (uterine tube or oviduct).
This is called ovulation. During this time the fimbriated end of the fallopian tube is applied to receive the ovum (Fig. 13). The ovum gradually travels through the fallopian tube.
Fertilization is internal and usually occurs in the upper one third part of the oviduct. During copulation the male sheds its sperms near the uterus, from there some sperms reach the fallopian tube. If an ovum is present there, one sperm enters the ovum. When the head of the sperm comes in contact with the corona radiata, its acrosome disintegrates (Fig. 14).
Normally, only one sperm enters an ovum. When the head of the sperm touches the ovum the cell membrane of the sperm and that of the ovum fuse and break to create a bridge of cytoplasm through which the rest of the sperm enters the ovum. Only head, neck and middle piece enter the ovum, the tail is left behind.
When the sperm enters, the chromosomes of the ovum split longitudinally and one half of each chromosome is then thrown out of the ovum. The halves to be thrown out and a little cytoplasm form a minute globular mass called the second polar body. After this the remaining halves grow to become regular chromosomes.
Now the mixing of chromosome occur and this is the process of fertilization completes. After fertilization the ovum is called a zygote.
The cleaving egg passes down the oviduct to reach the uterus where it would implant and complete its development by drawing its fundamental requirements from the uterine wall. As the cleaving eggs pass down the fallopian tubes, an albuminous coating is deposited around the outer surface of their zone pellucida. This albuminous layer forms an accessory egg layer similar to one deposited around the egg by oviduct cells in prototherian mammals, birds and reptiles.
Cleavage and Blastulation:
The fertilized eggs of eutherian mammals are microlecithal and minute in size. Cleavage of these eggs is of holoblastic type, due to a microlecithal condition the blastomeres tend to show size differences from the start. Moreover, the number of blastomeres do not increase by a regular doubling sequence but tend to show arithmetical progression.
Also, the overall speed of cleavage is much lower than in many animals. The slower rate is significant, as the cleavage in mammals preceeds at their body temperatures which are higher than ambient temperatures at which the development of the animals takes place.
The two cell stage is reached, 10-12 hours after fertilization. One of the two blastomeres remains slightly larger than the other. The larger cell divides first and thus forming three blastomeres, the smaller cell then divides to produce four cell stage in about 24 to 32 hours after fertilization. To reach the eight cell stage, one member of the larger blastomeres of four cell stage divides, forming the fine blastomeres producing a six cell stage (Fig. 15).
After a short period one of the smaller cell divides and thus, a total of seven blastomeres are formed. The last cleavage is followed by the division of the other smaller cell producing a eight cell stage. The mitotic spindles of each of these cleavages are formed at right angles to one another.
Thus showing an independence and asynchromy of cleavage. The rate of mitotic divisions increases and about 52.58 hours after fertilization the 16 cell stage is reached. The result of the successive cleavages is a solid mass of cells having 32 to 64 cells a morula. It is still surrounded by the zona pellucida, while the cells are dividing, the morula is also travelling towards the uterus, probably because of the peristalitic movement of the fallopian tube.
In the mean time, some fluid accumulates inside the morula to transform it into a blastocyst or blastodermic vesicle (or blastula), which is a spherical structure. The blastocyst has a wall composed of blastomeres, but it also has a small globular mass of blastomeres inside. These inner blastomeres is called the inner cell mass and the cavity around it is called the blastocyst cavity, which is filled with a fluid.
By about the seventh day after fertilization the blastocyst is composed of 58 to 64 blastomeres. At this stage the blastocyst enters the uterine cavity. Now the wall of the blastocyst is called the trophoblast which secretes the embryonic pole.
The blastocyst has the tendency to stick to any material tissue (for example, to the wall of the fallopian tube). To prevent this the zona pellucida layer remains till the blastocyst reaches the uterine cavity. In abnormal cases the blastocyst loses this layer earlier and sticks to the wall of the fallopian tube and starts developing. This is called tubal pregnancy. Such a blastocyst, however does not develop much further to form a regular embryo (Fig. 16).
During implantation the zona pellucida disappears and the trophoblast cells become giant and aggressively invade the uterine tissue to make contact by forming placenta. At this time, the inner cell mass under/goes progressive differentiation and eventually a layer of very flat cells appears on the interior surface of the inner cell mass (i.e. on the surface facing the blastocoelic cavity), that corresponds to the hypoblast of the chick and forms the future endoderm.
The remaining dorsal inner cell mass is called epiblast which has presumptive materials for ectoderm and mesoderm. The implantation becomes necessary for nourishment and further development of the blastocyst. The fully developed blastula is disc shaped hence called discoblastula.
It has an upper epiblast which contains cells for ectoderm and mesoderm and inner hypoblast which contains endodermal cells. These formative cells are ultimately encased by trophoblast (extra embryonic) cells and they form the roof of large fluid filled blastocoelic space.
Gastrulation:
In general, the method by which the single walled blastula becomes a double walled gastrula is called gastrulation. As a result of gastrulation the embryo acquires its two layers the upper layer is called ectoderm (epiblast) and the lower layer is called (hypoblast). The blastocyst cavity is referred to as primitive gut (archenteron).
At a later stage, folding process separates this primitive gut into a portion enclosed with in the embryonic body as the gut tract, and a distal sac communicating with the embryonic gut mid ventrally as the yolk sac. Mean/while, the mass of cells remaining after emigration of the endoderm cells of the primitive gut becomes more regularly arranged into a plate and is known as the embryonic disc.
A local differentiation occurs in the embryonic disc which presages the formation of the mesoderm. The mesodermal cells of posterior region of epiblast converage and accumulate to form the mid posterior thickening, the primitive streak. A Hensen’s node is seen at the anterior end of the primitive streak (Fig. 17).
The mesodermal cells soon involute through the primitive streak and diverge laterally and anteriorly and occupy position between epiblast and hypoblast. Epiblast also contributes some cells to endoderm (hypoblast) with the convergence and involution of more mesodermal and endodermal cells.
The size of the primitive streak increases, however the size of the primitive streak is shorter than the birds. The cells migrating forward from Hensen’s node remained packed more closely and give rise to the “Head process” the notoschordal rudiment.
The primitive streak in mammals, as in birds is a transient structure. Having giving rise to a mesodermal layer and the notochord rudiment, the primitive streak starts shrinking its anterior end with Hensen’s node receding farther and farther back, while in the anterior parts of the blastodisc the germinallayer enters the next phase of development, the neurulation.
During neurulation the neural ectoderm gets separated from the epidermal ectoderm and forms neural plate which invaginates to form the neural tube. The neural tube further differentiates into 5 brain regions and spinal cord. All the structures that arise from the neural tube and neural crest cells develop in a similar fashion as in the chick.
Side by side, the mesoderm differentiates into three portions, a middle epimere or somite, an intermediate mesomere and a lateral plate mesoderm. The hypomere the somites further differentiates into a dermatome which gives rise to the dermis of the skin, a sclerotome, which develops into axial skeleton, and a myotome which ultimately give rise to the striated musculature of the body.
The hypomere splits into an outer somatic mesodermal layer and an inner splanchnic mesodermal layer, both layers enclose an extra embryonic coelom and themselves forming extra embryonic membranes.
The somatic mesoderm and ectoderm together form the somatopleure, where as the splanchnic mesoderm and the underlying endoderm are collectively, called the splanchnopleure. The mesomere develops into both the reproductive and excretory structures.
The endoderm forms a primitive gut, in a similar manner as has been described in chick. The derivatives of the foregut are similar to those already described for the birds. The midgut development differs some what in terms of the establishment of extraembryonic membranes. The hind gut development in again similar to that seen in the birds.