In this article we will discuss about:- 1. Meaning of Electrocardiogram 2. Leads of Electrocardiogram 3. Electrocardiogram Trace 4. Sequence of Changes in Myocardial Infarction.
Meaning of Electrocardiogram (ECG):
At every beat, the heart is depolarized to trigger its contraction. This electrical activity is transmitted throughout the body and can be picked up on the skin. This is the principle behind the ECG. An ECG machine records this activity via electrodes on the skin and displays it graphically. An ECG involves attaching 10 electrical cables to the body, one to each limb and six across the chest.
ECG terminology has two meanings for the word “lead”:
i. The cable used to connect an electrode to the ECG recorder.
ii. The electrical view of the heart obtained from any one combination of electrodes.
The standard ECG uses 10 cables to obtain 12 electrical views of the heart. The different views reflect the angles at which electrodes “look” at the heart and the direction of the heart’s electrical depolarization.
Leads of Electrocardiogram (ECG):
I. Limb Leads:
Three bipolar leads and three unipolar leads are obtained from three electrodes attached to the left arm, the right arm, and the left leg, respectively. (An electrode is also attached to the right leg, but this is an earth electrode.)
The bipolar limb leads reflect the potential difference between two of the three limb electrodes:
i. The limb leads form the points of Einthoven’s triangle (an equilateral triangle used as a model of the standard limb leads used in electrocardiography).
ii. Einthoven’s law ― The potential differences between the bipolar leads measured simultaneously will have the values II = I + III.
iii. Lead I = LA ↔ RA, Lead II = LL ↔ RA, Lead III = LL ↔ LA (Fig. 6.17).
II. Augmented Limb Leads:
The unipolar leads reflect the potential difference between one of the three limb electrodes and an estimate of zero potential ― derived from the remaining two limb electrodes. These leads are known as augmented leads.
The augmented leads and their respective limb electrodes are:
i. aVR lead ― Right arm
ii. aVL lead ― Left arm
iii. aVF lead ― Left leg
III. Chest Leads:
Another six electrodes, placed in standard positions on the chest wall, give rise to a further six unipolar leads ― the chest leads (also known as precordial leads), V1-V6. The potential difference of a chest lead is recorded between the relevant chest electrode and an estimate of zero potential—derived from the average potential recorded from the three limb leads.
Placement of Electrodes:
Electrode label ― Electrode placement
RA ― On the right arm, avoiding bony prominences
LA ― In the same location that RA was placed, but on the left arm this time
RL ― On the right leg, avoiding bony prominences
LL ― In the same location that RL was placed, but on the left leg this time
V1 ― In the fourth intercostal space (between ribs 4 and 5) just to the right of the sternum
V2 ― In the fourth intercostal space (between ribs 4 and 5) just to the left of the sternum
V3 ― Between leads V2 and V4
V4 ― In the fifth intercostal space (between ribs 5 and 6) in the midclavicular line
V5 ― Horizontally even with V4, but in the anterior axillary line
V6 ― Horizontally even with V4 and V5 in the midaxillary line
Planes of View:
The limb leads looking at the heart in a vertical plane, whereas the chest leads look at the heart in a horizontal plane. In this way, a three-dimensional electrical picture of the heart is built up.
ECG leads and their respective views of the heart.
View ― Lead
Inferior ― II, III, aVF
Anterior ― I, aVL, V1–V3
Septal ― V3, V4
Lateral ― V4 –V6
The Electrocardiogram (ECG) Trace:
The ECG machine processes the signals picked up from the skin by electrodes and produces a graphic representation of the electrical activity of the patient’s heart.
The basic pattern of the ECG is logical:
i. Electrical activity towards a lead causes an upward deflection
ii. Electrical activity away from a lead causes a downward deflection
iii. Depolarization and repolarization deflections occur in opposite directions.
Normal Results:
Schematic representation of normal ECG. A typical ECG tracing of the cardiac cycle (heartbeat) consists of a P wave, a QRS complex, a T wave, and a U wave. The baseline voltage of the electrocardiogram is known as the isoelectric line.
Waves and Intervals:
i. P Wave:
It is due to atrial depolarization. Its duration is 0.1 sec and just precedes the atrial systole. Its amplitude is about 0.1-0.3 mV. The cardiac impulse reaches the AV node at the summit of P wave.
ii. QRS Complex:
The QRS complex reflects the rapid depolarization of the right and left ventricles. They have a large muscle mass compared to the atria and so the QRS complex usually has much larger amplitude than the P wave. Q wave is a small downward deflection which represents septal depolarization. R is a prominent positive wave and S is a small negative wave. Both R and S are due to depolarization of ventricular muscle. Duration of QRS complex is 0.08 sec and its amplitude is about 1 mV.
iii. T Wave:
It is due to the ventricular repolarization. It is a broad wave of variable duration and of low amplitude. Its duration is 0.27 sec and amplitude is about 0.15-0.5 mV.
iv. U Wave:
U Wave is rarely seen, and thought to possibly be the repolarization of the papillary muscles.
PR Interval:
PR interval is measured from the beginning of the P wave to the beginning of the QRS complex. The PR interval reflects the time the electrical impulse takes to travel from the sinus node through the AV node and entering the ventricles. The PR interval is therefore a good estimate of AV node function. The normal duration is 0.12-0.16 sec and does not exceed 0.2 sec. If it is more than 0.2 sec, it indicates conduction delay. PR interval corresponds to the A-C interval of the jugular pulse tracing.
QT Interval:
This is measured from the beginning of the QRS complex to the end of the T wave. The average duration is 0.4 sec. A prolonged QT interval is a risk factor for ventricular tachyarrhythmias and sudden death.
ST Interval:
The ST interval is measured from the J point to the end of the T wave. The average duration is 0.32 sec.
J Point:
The point at which the QRS complex finishes and the ST segment begins. Used to measure the degree of ST elevation or depression present.
ST Segment:
The ST segment connects the QRS complex and the T wave and it is isoelectric. Its duration is 0.05 sec.
Electrical Axis:
The heart’s electrical axis refers to the general direction of the heart’s depolarization wave front (or mean electrical vector) in the frontal plane. With a healthy conducting system the cardiac axis is related to where the major muscle bulk of the heart lies. Normally this is the left ventricle with some contribution from the right ventricle. It is usually oriented in a right shoulder to left leg direction, which corresponds to the left inferior quadrant of the hexaxial reference system, although -30° to +90° is considered to be normal.
If the left ventricle increases its activity or bulk then there is said to be “left axis deviation” as the axis swings round to the left beyond -30°, alternatively in conditions where the right ventricle is strained or hypertrophied then the axis swings round beyond +90° and “right axis deviation” is said to exist. Disorders of the conduction system of the heart can disturb the electrical axis without necessarily reflecting changes in muscle bulk.
Specific Arrhythmias:
i. Sinus Bradycardia:
Low sinus rate less than 60 beats/min.
ii. Sinus Tachycardia:
High sinus rate of 100-180 beats/min as occurs during exercise or other conditions that lead to increased SA nodal firing rate.
iii. Sick Sinus Syndrome:
A disturbance of SA nodal function that results in a markedly variable rhythm (cycles of bradycardia and tachycardia).
iv. Atrial Tachycardia:
A series of 3 or more consecutive atrial premature beats occurring at a frequency more than 100/min usually due to abnormal focus within the atria and paroxysmal in nature, therefore appearance of P wave is altered in different ECG leads. This type of rhythm includes paroxysmal atrial tachycardia (PAT).
v. Atrial Flutter:
Sinus rate of 250-350 beats/min.
vi. Atrial Fibrillation:
Uncoordinated atrial depolarizations.
vii. Junctional Escape Rhythm:
SA node suppression can result in AV node-generated rhythm of 40-60 beats/min (not preceded by P wave).
viii. AV Nodal Blocks:
A conduction block within the AV node (or occasionally in the bundle of His) that impairs impulse conduction from the atria to the ventricles.
First-Degree AV Nodal Block:
The conduction velocity is slowed so that the P-R interval is increased to greater than 0.2 seconds. It can be caused by enhanced vagal tone, digitalis, beta-blockers, calcium channel blockers, or ischemic damage.
Second-Degree AV Nodal Block:
The conduction velocity is slowed to the point where some impulses from the atria cannot pass through the AV node (Fig. 6.24). This can result in P waves that are not followed by QRS complexes. For example, 1 or 2 P waves may occur alone before one is followed by a QRS. When the QRS follows the P wave, the PR interval is increased. In this type of block, the ventricular rhythm will be less than the sinus rhythm.
There are two subtypes of second-degree AV blocks:
I. Mobitz I and
II. Mobitz II.
I. Mobitz I:
In Mobitz I (Wenkebach block), the PR interval gradually increases over several beats until it is sufficiently prolonged (that is, AV conduction is sufficiently impaired) that the impulse fails to pass into the ventricles (i.e. a P wave will not be followed by a QRS).
II. Mobitz II:
Mobitz II occurs when the PR interval is fixed in duration, but some P waves are not followed by a QRS (as illustrated). If complete heart block develops suddenly, there occurs a delay before ventricles start beating at their own rate. During this period the systemic blood pressure falls to a very low level and blood supply to brain becomes inadequate. If ventricular standstill lasts for few seconds, it causes dizziness, and fainting, called Stokes-Adams syndrome, or if it is more prolonged, it leads to loss of consciousness, convulsions and death.
Third-Degree AV Nodal Block:
Conduction through the AV node is completely blocked so that no impulses are able to be transmitted from the atria to the ventricles. QRS complexes will still occur (escape rhythm), but they will originate from within the AV node, bundle of His, or other ventricular regions. Therefore, QRS complexes will not be preceded by P waves.
Furthermore, there will be complete asynchrony between the P wave and QRS complexes. Atrial rhythm may be completely normal, but ventricular rhythm will be greatly reduced depending upon the location of the site generating the ventricular impulse. Ventricular rate typically range from 30 to 40 beats/ min.
i. Supraventricular Tachycardia (SVT):
Usually caused by re-entry currents within the atria or between ventricles and atria producing high heart rates of 140-250, the QRS complex is usually normal width, unless there are also intraventricular conduction blocks (e.g. bundle branch block).
ii. Ventricular Premature Beats (VPBs):
Caused by ectopic ventricular foci; characterized by widened QRS, often referred to as a premature ventricular complex, or PVC.
iii. Ventricular Tachycardia (VT):
High ventricular rate caused by aberrant ventricular automaticity (ventricular foci) or by intraventricular re-entry can be sustained or non-sustained (paroxysmal) usually characterized by widened QRS (>0.14 sec) rates of 100 to 280 beats/min, life-threatening.
iv. Ventricular Flutter:
Very rapid ventricular depolarizations >250/min, since wave appearance; leads to fibrillation.
v. Ventricular Fibrillation:
Uncoordinated ventricular depolarizations; leads to death if not quickly converted to a normal rhythm or at least a rhythm compatible with life.
Bundle Branch Block (BBB):
A problem in the bundle of His presents in an identical fashion to a combined block of both bundles, i.e. complete heart block. However, a more common occurrence is an isolated left or right bundle branch block. The patterns of the ECG are characteristic, but highly variable; the hallmark is a wide QRS complex. In left bundle branch block (LBBB), the pattern is best detected in V6 where there is an “M” pattern, while in V1 there is a “W” pattern.
In right bundle branch block (RBBB), the pattern is best detected in V1 where there is an RSR complex, while in V6 there is a QRS complex.
Ventricular Pre-Excitation:
Wolff-Parkinson-White syndrome (WPW syndrome) Pre-excitation is defined as an early depolarization of the ventricular myocardium that occurs prior to any conduction through the AV node. The most common condition in which this is seen is WPW syndrome, where there is an accessory AV pathway called the bundle of Kent.
The anomalous conducting system can be located anywhere around the mitral or tricuspid rings. Conduction through the accessory connection is faster and is independent of the heart rate. Consequently, the ventricular myocardium is activated from two directions – through the normal system and through the accessory pathway.
The resulting QRS complex is a product of fusion of the two distinct activation wave fronts. Since conduction over the accessory pathway is faster, the initial part of the QRS complex represents ventricular activation through this route (delta wave—Fig. 6.27).
Hyperkalemia:
Note the tall, tented T waves in ECG (Fig. 6.28).
Sequence of Electrocardiogram (ECG) Changes:
Sequence of Changes in Myocardial Infarction:
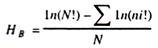
The ECG sequence shown in Fig. 6.29 gives you an idea as to how ST elevation would develop with this process of necrosis.
Image:
Sequence of changes in evolving anterior myocardial infarction.
Let’s work through the sequence in numerical order:
1. This picture shows a normal sinus complex. The ST segment is on the isoelectric line. At the onset of pain the ECG would be normal but the ST segment would soon start to change. In this picture, the T wave has grown taller.
2. Within an hour the ST segment would be noticeably elevated, indicating the onset on myocardial necrosis (tissue death).
3. If thrombolysis is administered, we would be looking for specific changes on the ECG. In this picture, the ST elevation has reduced by more than 50% from picture 2. You can also see the T wave invertion is much deeper. This is a good sign of reperfusion.
4. In this picture you can see the ST segment is back on the isoelectric line but the T wave remains inverted.
5. Six, in some cases, after a few months the ECG looks relatively normal. Compare picture 6 with picture 1. They look much the same but for the deep Q wave in picture 6. A deep Q wave is an indicator myocardial tissue death and will remain on the ECG.