The following points highlight the top six case histories of genetic diseases. The case histories are: 1. Xeroderma Pigmentosa 2. Myocardial Infarction 3. Duchenne Muscular Dystrophy 4. X-Linked Agammaglobulinemia 5. Diabetes Mellitus with Ketoacidosis 6. Acute Intoxication with Ethanol.
Case Histories of Genetic Diseases:
- Xeroderma Pigmentosa
- Myocardial Infarction
- Duchenne Muscular Dystrophy
- X-Linked Agammaglobulinemia
- Diabetes Mellitus with Ketoacidosis
- Acute Intoxication with Ethanol
Genetic Diseases: Case History # 1. Xeroderma Pigmentosa:
Classification: Physical exposure to UV irradiation
History and Physical Examination:
a. A 12-year old boy presented at Dermatology clinic with a skin tumor on his right cheek.
b. He had always avoided exposure to sunlight since it made his skin blister.
c. His skin had scattered areas of hyperpigmentation.
d. The dermatologist made a tentative diagnosis of xeroderma pigmentosa (pigmented dry skin).
Laboratory investigations:
a. Histologic examination of the excised tumor showed that it was a squamous carcinoma (a common type of skin cancer in older people, but not in a boy of this age).
b. A sample of skin was taken for the preparation of fibroblasts.
c. A research lab in radiobiology was set up to measure the amount of thymine dimers formed by exposure to UV light.
d. The patient’s fibroblasts and control fibroblasts were exposed to UV light and cell samples were taken at 8-hourly intervals for a total of 32 hours post-irradiation.
e. Extracts of DNA were prepared and the numbers of dimers remaining at each time point indicated were determined.
f. Only 24% of the dimers formed persisted in DNA extracted from the normal cells at 32 hours, about 95% were found in the extract from the patient’s cells at 32 hours.
This confirmed the diagnosis of xeroderma pigmentosa.
Comments:
a. Xeroderma pigmentosa (XP) is a relatively rare autosomal recessive condition in which the mechanisms for repair of DNA subsequent to damage inflicted by UV irradiation are impaired.
b. Thymine dimers are formed by the damage of DNA by UV irradiation. The covalent bonds are formed between carbons 5 and 5 and carbons 6 and 6 of adjacent intrachain thymine residues. These can be removed by an endonuclease. There is defect in this enzyme in XP.
c. In case, UV damage is not repaired, mutations in DNA will result and may cause cancer.
d. Patients with XP often suffer from variety of skin cancers from an early age.
e. The parents of this boy were advised that he would have to be watched throughout life for the development of new skin cancers.
f. The boy was advised to continue to avoid sunlight and to use an appropriate sunscreen ointment.
g. It has been estimated that patients with XP have a 1000-fold greater chance of developing skin cancer than do normal individuals.
Genetic Diseases: Case History # 2.
Myocardial Infarction:
Classification: Lack of oxygen History and Physical Examination:
a. A 46-year old businessman was admitted to the emergency department of his local hospital complaining of severe restrosternal pain for 2 hours.
b. He has previously been admitted to hospital once for treatment of a small myocardial infarction (MI), still he continued to smoke heavily.
c. His blood pressure was 150/90. Pulse 60/ min, and he was sweating continuously.
d. He was given morphine to relieve his pain and immediately transferred to a cardiac care unit, where ECG was started at once.
Laboratory tests:
a. The initial ECG showed S-T segment elevation and other changes in certain leads, indicative of an acute anterior trans-mural left ventricular infarction.
b. Blood was taken at 4 hours for measurement of the MB isozyme of CK. At 4 hours the activity of this isozyme was slightly increased and at 12 hours the elevation was 4-fold.
c. The plasma cholesterol was moderately elevated and triglyceride levels were normal.
Treatment:
a. The attending cardiologist decided to administer streptokinase (SK) by cardiac catheterization, because of the diagnosis of another trans-mural MI seen within 4 hours of the onset of symptoms.
b. Chest pain began to disappear after 12 hours and the patient felt comfortable.
c. He was discharged from hospital ten days later under the care of his family doctor with the advice to start a cholesterol lowering regimen and to stop smoking.
Discussion:
a. The decision was to limit the size of the infract by intracoronary administration of SK which can dissolve the thrombus.
b. For long term therapy, a drug was prescribed that inhibits HMG-CoA reductase to reduce the plasma cholesterol level.
c. The causes of atherosclerotic lesion in the coronary artery led to the thrombus. Atherosclerosis is caused by high levels of LDL, low levels of HDL, hypertension, high levels of cholesterol, and smoking. This patient had a high level of cholesterol and was a heavy smoker.
d. The lesion is now an intimal plaque. Hemorrhage and local inflammation can occur into the plaque leading to rupture of its surface. Platelets will adhere to the exposed collagen and a thrombus results.
e. In case, the thrombus persists 90% of the vessel wall, blood flow through the affected vessel may stop (total ischemia) and capillary hemoglobin will be depleted of oxygen very rapidly.
f. The affected myocardium shows the reduction of ATP, an accumulation of lactic acid, the development of severe acidosis, and a marked reduction in contractile force.
g. The accumulation of lactate and H+ inhibits glycolysis and thus stops ATP formation. Different studies have interpreted the depletion of ATP, activation of intracellular phospholipases (which can damage to cell membranes), activation of proteases, and accumulation of intracellular Ca++.
h. Irreversible damage of some cells had been made by one hour of complete ischemia. So administration of SK is a must.
i. Reperfusion injury can occur after the administration of SK. This can damage to the plasma membrane resulting in the entry of calcium ion from the plasma. High levels of intracellular Ca++ can pass inside the cell by activating or inhibiting various enzymes in an unregulated manner.
j. Superoxide may play a role in reperfusion injury.
The enzyme superoxide dismutase can convert superoxide to the less reactive hydrogen peroxide as shown below:
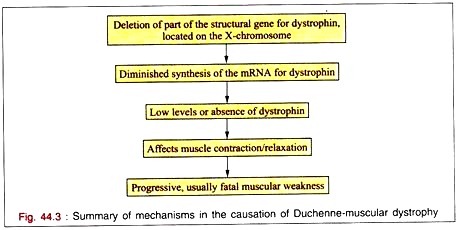
Genetic Diseases: Case History # 3.
Duchenne Muscular Dystrophy:
Classification: Genetic History and physical Examination:
a. A four-year old boy was brought to clinic at children’s hospital.
b. His mother had noticed that her son was walking awkwardly, and had difficulty climbing stairs.
c. His mother had a brother who died at the age of 19 of muscular dystrophy.
d. The physician noted muscle weakness in both the pelvic and shoulder girdle.
e. There was the modest enlargement of the calf muscle.
f. The pediatrician made a tentative diagnosis of Duchenne muscular dystrophy (DMD) due to the patients’ muscle weakness and its distribution.
Lab and other tests:
a. Serum creatine phosphokinase activity was markedly increased.
b. Electromyographic findings showed muscular dystrophy.
c. Nerve conduction studies were normal.
d. A biopsy of calf muscle showed areas of muscle necrosis and some variation in the size of muscle fibres.
e. Muscle biopsy by electrophoresis showed an absence of the protein dystrophin.
Discussion:
a. The lab findings confirmed the pediatrician’s provisional diagnosis of DMD.
b. This is severe X-chromosome-linked degenerative disease of muscle.
c. This happens 1 in 3500 live male births.
d. It affects young boys who show loss of strength in their proximal muscles leading to difficulty in standing up and to very severe weakness.
e. There had been the defect to the middle of the short arm of the X-chromosome and to subsequent identification of a segment of DNA that was deleted in patients with DMD.
f. Antibodies against dystrophin were located in the sarcolemma (plasma membrane) of normal muscle and was absent in the sarcolemma of patients with DMD.
g. Further studies have shown that the gene coding for dystrophin is one of the largest human genes recognized to date.
h. Dystrophins are being produced by recombinant DNA technology. The availability of cDNA probes for dystrophin facilitates prenatal diagnosis of DMD by chorionic villus sampling.
i. The demonstration of dystrophin as a cause of DMD is one of the major accomplishments of the application of the new molecular biology to human disease.
Treatment:
a. The boy was encouraged to exercise, and regular attendance at a specialized muscular dystrophy clinic was started for the treatment of the complications if arose.
b. The mother was advised to take genetic instruction.
Genetic Diseases: Case History # 4.
X-Linked Agammaglobulinemia:
Classification: Immunologic, genetic History and Physical Examination:
a. A-3-year old boy was referred to children’s hospital with a high temperature, pain in the chest, and difficulty in breathing.
b. His family doctor diagnosed pneumonia.
c. Since his older brother had previously been diagnosed as having X-linked agammaglobulinemia, the attack of pneumonia raised the suspicion that the younger brother might also lack the potential to synthesize gamma globulins.
Lab Results:
a. Electrophoretic analysis showed the levels of albumin and α- and β-globulins normal, but only a trace of γ-globulins was detected.
b. B lymphocytes were markedly low in the blood but the T-cell count was normal.
c. A biopsy of lymph node showed an absence of plasma cells.
d. Streptococcus pneumoniae was demonstrated in samples of sputum.
Discussion:
a. Disorders of the immune system can affect either the B-cell system(circulating immunoglobulin’s) or the T-cell system (cell-mediated immune responses).
b. This is an immunologic condition, although the underlying cause is genetic.
c. X-linked agammaglobulinemia affects young boys and is a Relatively uncommon condition.
d. The actual nature of the defect in this condition has not been established but involves the X-chromosomes.
e. Although only a few circulating B cells are present, normal numbers of pre-B cells are present in bone narrow.
Genetic Diseases: Case History # 5.
Diabetes Mellitus with Ketoacidosis:
Classification: Endocrine deficiency, Lack of Insulin History and physical examination:
a. A 14-year old girl was admitted to children’s hospital in coma.
b. She developed a sore throat and fever two weeks before according to her mother’s statement.
c. Some days before admission, she began to complain of thirst and started to get up several times during the night for urination.
d. On the day of admission the girl had started to vomit.
e. On examination she was dehydrated, her skin was cold, she was deeply breathing, and her breath had a fruity odour.
f. Her blood pressure was 90/60 mm of Hg. and her pulse rate was 115/min.
g. A diagnosis of severe type I insulin-dependent diabetes mellitus with resulting ketoacidosis and coma was made by the intern on duty.
Lab results:
Treatment:
a. In the treatment of diabetic Ketoacidosis (DKA), Insulin administration and saline fluids are most essential. The patient was given insulin (10 µ/h) added to 0.9% NaCl. Glucose was withheld until the level of plasma glucose fell below 250 mg/dl.
b. KCL was also administered very cautiously, continuous checking of K levels is very important in the management of DKA, because insufficient management of K balance is the major cause of death in this condition.
c. Bicarbonate may be necessary if acidosis is very severe.
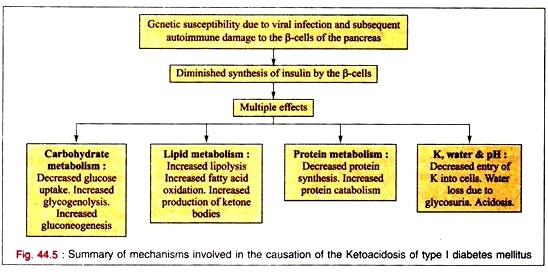
Discussion:
a. This type of diabetic patients have a genetic susceptibility, which may be due to a viral infection.
b. The infection and consequent inflammatory reaction may alter the antigenicity of the surface of the pancreatic β-cells and establish an autoimmune reaction involving cytotoxic antibodies and T lymphocytes. This causes destruction of p-cells resulting in type I diabetes mellitus.
c. The sore throat that the patient had several weeks before reflected the initiating viral infection.
d. The low pH indicated a severe acidosis due to the increased production of acetoacetic acid and β-hydroxybutyric acid.
e. The levels of urea and creatinine indicated some renal impairment, dehydration, and increased catabolism of protein.
f. A high plasma potassium level is often found in DKA due to the lowered uptake of potassium by cells in the absence of insulin.
g. The increased osmolality of plasma due to hyperglycemia causes the development of coma in DKA.
Genetic Diseases: Case History # 6.
Acute Intoxication with Ethanol:
Classification: Chemical History and Physical Examination:
a. A 52-year old male was admitted to the emergency department in coma.
b. He had been a moderate drinker before the death of his wife. After her death he had become depressed and started increasing alcohol consumption. He had been eating poorly.
c. On Sunday morning his married daughter found him unconscious on the living room couch.
d. His breathing was deep and noisy, alcohol could be smelled on his breath, and his temperature was 35.5°C (normal 37.4)
e. The diagnosis on admission was coma due to excessive alcohol intake.
Lob tests:
Blood results:
Alcohol : 500 mg/dL
Glucose : 2.7 mmol/L (normal 3.6-6.1)
Lactate : 8.0 mmol/L (normal 0.5-2.22)
pH : 7.21 (normal 7.4)
Treatment:
a. Hemodialysis was immediately started to eliminate the toxic ethanol from the body due to high level of blood alcohol and the coma.
b. The level of blood alcohol fell rapidly and the patient became conscious.
c. Intravenous glucose (5%) was administered after dialysis was stopped to counteract the hypoglycemia.
d. The patient made a good recovery and was referred to for psychiatric advice.
Discussion:
a. The remarkable problem is the development of liver cirrhosis in individuals who are accustomed to high intake of ethanol (e.g., 80 gm. of ethanol daily) for more than 10 years.
b. In the liver, ethanol is converted to acetate through acetaldehyde by alcohol dehydrogenase and acetaldehyde dehydrogenase. Acetate is then converted to acetyl-CoA. Reduced NAD is formed in both these reactions.
c. High levels of reduced NAD favour the formation of lactate from pyruvate resulting in lactic acidosis.
d. The diminished pyruvate concentration inhibits gluconeogenesis.
e. In severe cases, liver glycogen level is diminished and hypoglycemia results due to non-availability of glycogenolysis.
f. The microsomal cytochrome P-450 also produces acetaldehyde which is a highly reactive molecule and can form adducts with proteins, nucleic acids, and other molecules. The ability of acetaldehyde to react with various molecules is involved in the causation of the toxic effects of ethanol.
g. The biological membranes are affected by ethanol and are excitable by that affect. This results in alterations of their action potentials, and also affects neurotransmitter release.
h. All of these depress cerebral function and, if severe enough, can produce coma and death from respiratory paralysis.