Read this article to learn about the production, advantages and limitations of monoclonal antibodies.
Antibodies or immunoglobulin’s are protein molecules produced by a specialized group of cells called B-lymphocytes (plasma cells) in mammals. The structures, characteristics and various other aspects of immunoglobulin’s (Igs) are described elsewhere. Antibodies are a part of the defense system to protect the body against the invading foreign substances namely antigens.
Each antigen has specific antigen determinants (epitopes) located on it. The antibodies have complementary determining regions (CDRs) which are mainly responsible for the antibody specificity. In response to an antigen (with several different epitopes), B-lymphocytes gear up and produce many different antibodies. These types of antibodies which can react with the same antigen are designated as polyclonal antibodies.
The polyclonal antibody production is variable and is dependent on factors such as epitopes, response to immunity etc. Due to lack of specificity and heterogenic nature, there are several limitations on the utility of polyclonal antibodies for therapeutic and diagnostic purposes.
Monoclonal antibody (MAb) is a single type of antibody that is directed against a specific antigenic determinant (epitope). It was a dream of scientists to produce MAbs for different antigens. In the early years, animals were immunized against a specific antigen, B-lymphocytes were isolated and cultured in vitro for producing MAbs. This approach was not successful since culturing normal B-lymphocytes is difficult, and the synthesis of MAb was short-lived and very limited.
It is interesting that immortal monoclonal antibody producing cells do exist in nature. They are found in the patients suffering from a disease called multiple myeloma (a cancer of B- lymphocytes). It was in 1975. George Kohler and Cesar Milstein (Nobel Prize, 1984) achieved large scale production of MAbs. They could successfully hybridize antibody—producing B-lymphocytes with myeloma cells in vitro and create a hybridoma.
The result is that the artificially immortalized B-lymphocytes can multiply indefinitely in vitro and produce MAbs. The hybridoma cells possess the growth and multiplying properties of myeloma cells but secrete antibody of B-lymphocytes. The production of monoclonal antibodies by the hybrid cells is referred to as hybridoma technology.
Contents
- Principle for Creation of Hybridoma Cells:
- Production of Monoclonal Antibodies:
- Large Scale Production of MAbs:
- Human Monoclonal Antibodies:
- Genetic Engineering Strategies for the Production of Human- Mouse MAbs:
- Production of Mabs in E. coli:
- Second Generation Monoclonal Antibodies:
- Advantages of Monoclonal Antibodies:
- Limitations of Monoclonal Antibodies:
Principle for Creation of Hybridoma Cells:
The myeloma cells used in hybridoma technology must not be capable of synthesizing their own antibodies. The selection of hybridoma cells is based on inhibiting the nucleotide (consequently the DNA) synthesizing machinery. The mammalian cells can synthesize nucleotides by two pathways—de novo synthesis and salvage pathway (Fig. 17.1).
The de novo synthesis of nucleotides requires tetrahydrofolate which is formed from dihydrofolate. The formation of tetrahydrofolate (and therefore nucleotides) can be blocked by the inhibitor aminopterin. The salvage pathway involves the direct conversion of purines and pyrimidine’s into the corresponding nucleotides. Hypoxanthine guanine phosphoribosyl transferase (HGPRT) is a key enzyme in the salvage pathway of purines.
It converts hypoxanthine and guanine respectively to inosine monophosphate and guanosine monophosphate. Thymidine kinase (TK), involved in the salvage pathway of pyrimidine’s converts thymidine to thymidine monophosphate (TMP). Any mutation in either one of the enzymes (HGPRT or TK) blocks the salvage pathway.
When cells deficient (mutated cells) in HGPRT are grown in a medium containing hypoxanthine aminopterin and Thymidine (HAT medium), they cannot survive due to inhibition of de novo synthesis of purine nucleotides (Note : Salvage pathway is not operative due to lack of HGPRT). Thus, cells lacking HGPRT, grown in HAT medium die.
The hybridoma cells possess the ability of myeloma cells to grow in vitro with a functional HGPRT gene obtained from lymphocytes (with which myeloma cells are fused). Thus, only the hybridoma cells can proliferate in HAT medium, and this procedure is successfully used for their selection.
Production of Monoclonal Antibodies:
The establishment of hybridomas and production of MAbs involves the following steps (Fig. 17.2).
1. Immunization
2. Cell fusion
3. Selection of hybridomas
4. Screening the products
5. Cloning and propagation
6. Characterization and storage.
1. Immunization:
The very first step in hybridoma technology is to immunize an animal (usually a mouse), with appropriate antigen. The antigen, along with an adjuvant like Freund’s complete or incomplete adjuvant is injected subcutaneously (adjuvants are non-specific potentiators of specific immune responses). The injections at multiple sites are repeated several times.
This enables increased stimulation of B-lymphocytes which are responding to the antigen. Three days prior to killing of the animal, a final dose of antigen is intravenously administered. The immune-stimulated cells for synthesis of antibodies have grown maximally by this approach. The concentration of the desired antibodies is assayed in the serum of the animal at frequent intervals during the course of immunization.
When the serum concentration of the antibodies is optimal, the animal is sacrificed. The spleen is aseptically removed and disrupted by mechanical or enzymatic methods to release the cells. The lymphocytes of the spleen are separated from the rest of the cells by density gradient centrifugation.
2. Cell Fusion:
The thoroughly washed lymphocytes are mixed with HGPRT defective myeloma cells. The mixture of cells is exposed to polyethylene glycol (PEG) for a short period (a few minutes), since it is toxic. PEG is removed by washing and the cells are kept in a fresh medium. These cells are composed of a mixture of hybridomas (fused cells), free myeloma cells and free lymphocytes.
3. Selection of Hybridomas:
When the cells are cultured in HAT medium (the principle described above), only the hybridoma cells grow, while the rest will slowly disappear. This happens in 7-10 days of culture. Selection of a single antibody producing hybrid cells is very important. This is possible if the hybridomas are isolated and grown individually. The suspension of hybridoma cells is so diluted that the individual aliquots contain on an average one cell each. These cells, when grown in a regular culture medium, produce the desired antibody.
4. Screening the Products:
The hybridomas must be screened for the secretion of the antibody of desired specificity. The culture medium from each hybridoma culture is periodically tested for the desired antibody specificity. The two techniques namely ELISA and RIA are commonly used for this purpose.
In both the assays, the antibody binds to the specific antigen (usually coated to plastic plates) and the unbound antibody and other components of the medium can be washed off. Thus, the hybridoma cells producing the desired antibody can be identified by screening. The antibody secreted by the hybrid cells is referred to as monoclonal antibody.
5. Cloning and Propagation:
The single hybrid cells producing the desired antibody are isolated and cloned. Two techniques are commonly employed for cloning hybrid cells-limiting dilution method and soft agar method.
Limiting dilution method:
In this procedure, the suspension of hybridoma cells is serially diluted and the aliquots of each dilution are put into micro culture wells. The dilutions are so made that each aliquot in a well contains only a single hybrid cell. This ensures that the antibody produced is monoclonal.
Soft agar method:
In this technique, the hybridoma cells are cultured in soft agar. It is possible to simultaneously grow many cells in semisolid medium to form colonies. These colonies will be monoclonal in nature. In actual practice, both the above techniques are combined and used for maximal production of MAbs.
6. Characterization and Storage:
The monoclonal antibody has to be subjected to biochemical and biophysical characterization for the desired specificity. It is also important to elucidate the MAb for the immunoglobulin class or sub-class, the epitope for which it is specific and the number of binding sites it possesses.
The stability of the cell lines and the MAbs are important. The cells (and MAbs) must be characterized for their ability to withstand freezing, and thawing. The desired cell lines are frozen in liquid nitrogen at several stages of cloning and culture.
Large Scale Production of MAbs:
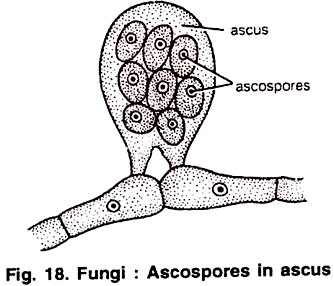
The production MAbs in the culture bottles is rather low (5-10 (ig/ml). The yield can be increased by growing the hybrid cells as ascites in the peritoneal cavity of mice. The ascitic fluid contains about 5-20 mg of MAb/ml. This is far superior than the in vitro cultivation techniques.
But collection of MAb from ascitic fluid is associated with the heavy risk of contamination by pathogenic organisms of the animal. In addition, several animals have to be sacrificed to produce MAb. Hence, many workers prefer in vitro techniques rather than the use of animals.
Encapsulated hybridoma cells for commercial production of MAbs:
The yield of MAb production can be substantially increased by increasing the hybridoma cell density in suspension culture. This can be done by encapsulating the hybridomas in alginate gels and using a coating solution containing poly-lysine (Fig. 17.3). These gels allow the nutrients to enter in and antibodies to come out.
By this approach, a much higher concentration of MAb production (10-100 µg/ml) can be achieved. Damon Biotech Company and Cell-Tech use encapsulated hybridoma cells for large-scale production of MAbs. They employ 100-liter fermenters to yield about 100g of MAbs in about 2 weeks period.
Human Monoclonal Antibodies:
The monoclonal antibodies produced by using mice are quite suitable for in vitro use. However, their administration to humans is associated with immunological complications, since they are foreign to human body. Production of human monoclonal antibodies is preferred. However, it is difficult to produce human MAbs by conventional hybridoma technology.
The following are the major limitations:
i. For ethical reasons, humans cannot be immunized against antigens.
ii. The fused human lymphocyte-mouse myeloma cells are very unstable.
iii. There are no suitable myeloma cells in humans that can replace mouse myeloma cells.
For the above reasons, alternative arrangements are made to produce human MAbs. These are briefly described below.
Viral transformation of human B-lymphocytes:
B-Lymphocytes, actively synthesizing antibody, are treated with fluorescent-labeled antigen. The fluorescent-activated cells are separated. However, B-cells on their own, cannot grow in culture. This limitation can be overcome by transforming B-lymphocytes with Epstein-Bar virus (EBV). Some of the EBV-transformed cells can grow in culture and produce monoclonal antibodies. Unfortunately, the yield of MAb is very low by this approach.
SCID mouse for producing human MAbs:
The mouse suffering from severe combined immunodeficiency (SCID) disease lacks its natural immunological system. Such mouse can be challenged with appropriate antigens to produce human MAbs.
Transgenic mouse for producing human MAbs:
Attempts have been made in recent years to introduce human immunoglobulin genes into the mice to develop transgenic mice. Such mice are capable of synthesizing human immunoglobulin’s when immunized to a particular antigen. The B-lymphocytes isolated from transgenic mice can be used to produce MAbs by the standard hybridoma technology. The above three approaches are quite laborious, and the yield of human MAbs is very low. Consequently, researchers continue their search for better alternatives.
Genetic Engineering Strategies for the Production of Human- Mouse MAbs:
With the advances in genetic engineering, it is now possible to add certain human segments to a mouse antibody. This is truly a hybridized antibody and is referred to as humanized antibody or chimeric antibody.
Substitution of Fv region of human Ig by mouse Fv:
The DNA coding sequences for Fv regions of both L and H chains of human immunoglobulin are replaced by Fv DNA sequence (for L and H chains) from a mouse monoclonal antibody (Fig. 17.4A). The newly developed humanized MAb has Fc region of Ig being human. This stimulates proper immunological response. The chimeric antibodies produced in this manner were found to be effective for the destruction of tumor cells in vitro.
Substitution of Human Ig by Mouse CDRs:
Genetic engineers have been successful in developing human MAbs containing mouse complementary determining regions (CDRs). This is made possible by replacing CDRs genes (CDR1, CDR2, and CDR3) of humans by that of mouse. These chimeric antibodies (Fig. 17.4B) possess the antigen binding affinities of the mouse and they can serve as effective therapeutic agents. So far, about 50 monoclonal antibodies have been produced by this approach. However, this technique is costly and time consuming.
Bi-specific monoclonal antibodies:
The MAbs in which the two arms of Fab (antigen-binding) have two different specificities for two different epitopes are referred to as bi-specific MAbs. They may be produced by fusing two different hybridoma cell lines (Fig. 17.5) or by genetic engineering. Bi-specific Fab MAbs theoretically, are useful for a simultaneous and combined treatment of two different diseases.
Production of Mabs in E. coli:
The hybridoma technology is very laborious, expensive and time consuming. To overcome these limitation, researchers have been trying to genetically engineer bacteria, plants and animals. The objective is to develop bioreactors for the large scale production of monoclonal antibodies.
It may be noted that the antigen binding regions of antibody (Fv or Fab fragments) are very crucial, while the Fc portion is dispensable. A schematic representation of the procedure adopted for the production of functional antibody fragments is shown in Fig. 17.6, and is briefly described.
The mRNA from isolated B-lymphocytes of either human or mouse is converted to cDNA. The H and L chain sequences of this cDNA are amplified by PCR. The so produced cDNAs are then cut by restriction endonucleases. H and L chain sequences are separately cloned in bacteriophage vectors.
These sequences are put together and cloned in another bacteriophage vector. The combined H and L chains (forming Fv fragment) are screened for antigen binding activity. The specific H and L chains forming a part of the plasmid are transformed in E. coli. These E. coli, in turn, can be harvested to produce Fv fragments to bind to specific antigens.
Second Generation Monoclonal Antibodies:
In the recent years, a number of improvements have been made to produce more specific, sensitive and desired MAbs. This has been possible due to the rapid advances made in genetic engineering techniques. For instances, by employing site- directed mutagenesis, it is possible to introduce cysteine residues at the predetermined positions on the MAb. These cysteine residues which facilitate the isotope labeling may be more useful in diagnostic imaging and radio-immunotherapy.
Advantages of Monoclonal Antibodies:
Monoclonal antibodies truly represent a homogeneous state of a single molecular species. Each MAb is specific to a given antigenic determinant. This is in contrast to the conventional antiserum that contains polyclonal antibodies. The wide range of applications of MAbs is described later.
Limitations of Monoclonal Antibodies:
Hybridoma technology is laborious and time consuming. MAbs are produced against a single antigenic determinant; therefore, they cannot differentiate the molecule as a whole. Sometimes, they may be incapable of distinguishing groups of different molecules also.
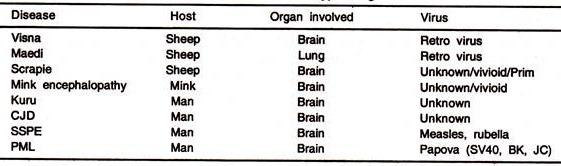
The presence of retroviruses as a part of the mammalian chromosomes is a common occurrence. Mice used in MAb production carry several viruses (adenovirus, hepatic virus, retrovirus, reovirus, cytomegalovirus, thymic virus). The presence of some of these viruses has been detected in the hybridomas.
This poses a great danger, since there is no guarantee that MAb produced is totally virus-free, despite the purification. For this reason, US Food and Drug Administration insists that MAb for human use should be totally free from all pathogenic organisms, including viruses.